UnitedHealthcare Medicare Advantage Plans in Utah for 2026
Curious about the potential UnitedHealthcare Medicare Advantage plans in Utah for 2026? This article breaks down the available plan types, potential benefits, and the enrollment process, so you can make an informed decision.
Key Takeaways
- Some of UnitedHealthcare’s Medicare Advantage plans in Utah for 2026 may offer a comprehensive range of benefits, which might include additional dental, vision, and hearing coverage, likely tailored to meet the diverse needs of beneficiaries.
- Eligibility for enrollment requires meeting Original Medicare specifications and residing within the service area, with specific criteria for Special Needs and Dual Special Needs Plans.
- Possible changes might include lower out-of-pocket costs for certain prescription drugs and the potential elimination of the donut hole, which could enhance affordability and possibly offer financial relief for members, especially for those with chronic conditions.
Compare Plans in One Step!
Enter Zip Code
Overview of UnitedHealthcare Medicare Advantage Plans in Utah

UnitedHealthcare’s Medicare Advantage plans in Utah for 2026 may offer a comprehensive suite of benefits designed to meet the diverse needs of Medicare beneficiaries. Some plans might integrate coverage for dental, hearing, and vision services, possibly ensuring that members could receive complete healthcare support in one package. The stability of these plans will likely be backed by renewal contracts with Medicare, which means that members could count on consistent service and coverage options year after year.
These plans will likely be designed with flexibility, catering to the specific needs of the Utah population. Whether you are looking for comprehensive medical coverage or potential benefits, UnitedHealthcare’s Medicare Advantage plans could offer a variety of options to suit different preferences and health requirements. This could potentially ensure that Medicare beneficiaries in Utah have access to tailored healthcare solutions that enhance their quality of life.
Possible Coverage Options
Certain UnitedHealthcare Medicare Advantage plans may be known for their potential coverage options, which could potentially offer members with comprehensive health benefits that might go beyond standard Medicare coverage. Some plans may offer vision coverage, which may include an annual eye examination and a financial allowance for purchasing contact lenses or frames. Routine standard lenses, such as single, bifocal, trifocal, or standard progressive lenses, may be fully covered either annually or every two years, possibly ensuring that members could maintain optimal eye health without incurring hefty out-of-pocket costs.
Hearing services could be another potential benefits. Members will likely have access to hearing aid services through a network provider, which may include hearing exams and various hearing aid options within the UnitedHealthcare network. This could facilitate addressing hearing issues, common with age, possibly improving overall quality of life.
Certain plans may also offer robust dental coverage, although it may vary depending on whether members choose in-network or out-of-network providers. In-network services typically come with lower out-of-pocket costs, possibly making it advantageous for members to utilize UnitedHealthcare’s extensive network of dental professionals.
Potential Prescription Drug Benefits

Some UnitedHealthcare plans may integrate prescription drug coverage, which could potentially provide significant financial relief for members. This coverage may offer a maximum out-of-pocket expense for certain Medicare-covered medications, possibly ensuring members don’t face further copayment or coinsurance costs once this limit is reached.
The possible elimination the coverage gap, commonly known as the donut hole, could be another advantage. This potential change could mean that Medicare beneficiaries might not experience a sudden increase in out-of-pocket costs for some prescription drugs after reaching a certain spending threshold. Cost-sharing may remain consistent, likely making it easier for members to budget for their medications.
Special Programs for Chronically Ill Enrollees
For chronically ill enrollees, UnitedHealthcare Medicare Advantage plans might offer specialized programs designed to provide additional support and resources. These programs could be particularly beneficial for individuals with conditions such as cardiovascular disease and heart disease, possibly offering tailored health benefits that could help manage their medical conditions.
These special programs will likely provide access to a range of resources and support services. This could include not only medical care but also educational resources and wellness programs that could empower members to take an active role in managing their health. Addressing the unique needs of chronically ill members, UnitedHealthcare’s Medicare Advantage plans will likely help improve health outcomes and enhance the quality of life.
Enrollment Process and Eligibility Requirements
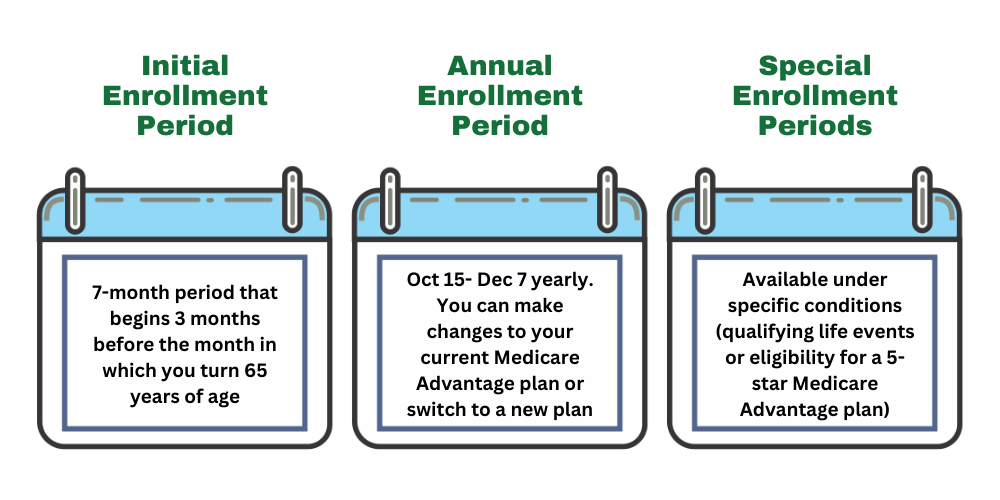
Enrolling in UnitedHealthcare Medicare Advantage plans in Utah requires understanding the eligibility requirements and the enrollment process. Typically, individuals must be enrolled in Medicare Part A and Part B to be eligible for these plans. Additionally, specific criteria may apply for Dual Special Needs Plans (D-SNPs), which require both Medicare and Medicaid enrollment.
The Medicare Open Enrollment Period, which runs from October 15 to December 7 each year, is the primary time for beneficiaries to enroll, switch, or drop their Medicare Advantage plans. Outside of this period, special enrollment periods may be available based on certain qualifying events, allowing for enrollment changes when necessary. Beneficiaries need to understand these timelines to ensure they can make the necessary adjustments to their coverage.
Potential Cost and Payment Options
Understanding the potential costs and payment options associated with Medicare Advantage plans could be vital for managing healthcare expenses. Some UnitedHealthcare plans may include an out-of-pocket maximum, which could potentially alleviate the financial burden on members, possibly making healthcare more affordable.
Additionally, certain copay structures within some plans may be tiered, meaning that not all medications will be eligible for the lowest copay rates. Understanding these tiers and how they might apply to specific medications will likely be essential for budgeting healthcare costs. With various payment options, UnitedHealthcare likely ensures its members can access necessary healthcare services without undue financial strain.
Comparison with Other Medicare Advantage Plans
Several factors might stand out when comparing UnitedHealthcare Medicare Advantage plans to other options available in Utah. First, some Medicare Advantage plans, including those from UnitedHealthcare, may charge a lower premium apart from the standard Part B premium, which could be an attractive feature for enrollees. Additionally, certain plans may also offer an out-of-pocket spending limit, which could offer financial protection that traditional Medicare does not.
UnitedHealthcare has been a major player in the Medicare Advantage market, which will likely influence overall cost structures and payment options. The extensive provider networks offered by UnitedHealthcare might exceed those of other providers, possibly allowing for better access to healthcare services. This could be particularly beneficial in managing out-of-pocket expenses.
However, it’s essential to review the details of each plan carefully, as some Medicare Advantage plans may have limitations or exclusions that affect coverage. Understanding these differences could help beneficiaries choose the plan that best meets their healthcare needs.
Summary
The UnitedHealthcare Medicare Advantage plans in Utah for 2026 will likely offer a wide range of benefits designed to meet the diverse needs of Medicare beneficiaries. From potential benefits for vision, hearing, and dental services and sometimes prescription drug benefits, to improved access to Medicaid services, these plans could provide robust support for maintaining overall health and well-being. The special programs for chronically ill enrollees and the dedicated customer service resources may further enhance the value of these plans.
The enrollment process is straightforward, with specific eligibility requirements and multiple enrollment periods ensuring that beneficiaries can access the coverage they need. Cost and payment options will likely be designed to be flexible and manageable, helping members navigate their healthcare expenses effectively. When compared to other Medicare Advantage plans, UnitedHealthcare may stand out for its extensive provider networks and advantageous copayment structures.
Overall, UnitedHealthcare Medicare Advantage plans in Utah for 2026 could present a compelling option for Medicare beneficiaries seeking comprehensive, affordable, and accessible healthcare coverage.
Frequently Asked Questions
→ What are the potential features of UnitedHealthcare Medicare Advantage plans in Utah for 2026?
Some UnitedHealthcare Medicare Advantage plans in Utah might include comprehensive coverage, such as dental, hearing, and vision services, and sometimes prescription drug coverage. These potential features could ensure that you have access to essential healthcare services tailored to your needs.
→ What special programs are available for chronically ill enrollees?
UnitedHealthcare will likely provide specialized programs for chronically ill enrollees. These programs are designed to support better health outcomes and improve quality of life.
→ How could the Inflation Reduction Act impact Medicare Advantage plans?
Unfortunately, the plan details for 2026 have not been released, but make sure to check back in to this article/website for updated information for the 2026 calendar year.
→ What are the enrollment periods and eligibility requirements for these plans?
You can enroll in Medicare plans during the Open Enrollment Period from October 15 to December 7, with additional special enrollment periods for specific qualifying events. Generally, you must be enrolled in Medicare Part A and Part B to qualify.

ZRN Health & Financial Services, LLC, a Texas limited liability company



