Secure Horizons Medicare Advantage Plans 2026
Curious about the potential Secure Horizons Medicare Advantage Plans for 2026? This guide explores the potential features, available coverage, and how these plans could benefit you.
Key Takeaways
- Secure Horizons Medicare Advantage Plans will likely provide comprehensive and tailored coverage, which could include integrated prescription drug benefits.
- Available plan types include HMO, PPO, and Special Needs Plans (SNPs), each designed to address specific healthcare needs and preferences of Medicare beneficiaries.
- Enrollment periods for these plans include the annual election period from October 15 to December 7, along with new Monthly Special Enrollment Period options, enhancing beneficiary flexibility.
Compare Plans in One Step!
Enter Zip Code
Understanding Secure Horizons Medicare Advantage Plans

Secure Horizons Medicare Advantage Plans will likely aim to offer comprehensive coverage tailored to diverse consumer needs. These plans have been designed to provide stability and potentially broaden access to essential healthcare services for Medicare beneficiaries.
Moreover, these plans will likely emphasize tailored benefits for individuals managing chronic conditions, possibly facilitating better health outcomes.
Types of Secure Horizons Medicare Advantage Plans Available
The Secure Horizons Medicare Advantage lineup includes diverse plan types tailored to meet the needs of various Medicare beneficiaries. These include Health Maintenance Organization (HMO) plans, Preferred Provider Organization (PPO) plans, and Special Needs Plans (SNPs). Each type offers unique benefits and coverage options, potentially ensuring that there could be a plan suited for every individual’s specific healthcare needs.

HMO Plans
HMO plans often provide lower costs than other types, requiring members to use a network of doctors and obtain referrals for specialist care. Members must choose a primary care physician (PCP) and get referrals to see specialists, which helps coordinate care and manage overall healthcare costs. HMO plans may also include lower out-of-pocket cost limits for certain prescription drugs, possibly enhancing affordability for members.
Many HMO plans will offer integrated care options for members with both Medicare and Medicaid, improving coordination of benefits. This integration could be particularly beneficial for those managing chronic conditions, as it will likely streamline care and ensures that various aspects of a member’s health are addressed.
However, HMO plans generally provide a more limited network of doctors and hospitals compared to some other Medicare Advantage options.
PPO Plans
PPO plans offer greater flexibility, allowing members to see any healthcare provider without needing a referral, though costs may be higher for out-of-network services. Members can receive care from both in-network and out-of-network providers, possibly making PPO plans a good choice for those who want more freedom in choosing their healthcare providers.
These plans might include additional benefits such as vision and dental coverage beyond what Original Medicare offers. However, the increased flexibility may also come with higher premiums compared to HMO plans. Despite the higher costs, many find the ability to see specialists without referrals and use out-of-network providers worth the extra expense.
Special Needs Plans (SNPs)
Special Needs Plans (SNPs) are specifically designed to cater to individuals with particular health needs, offering customized benefits and services for those eligible. These plans are tailored for specific groups of people, including those with chronic conditions, offering coordinated care and additional services relevant to their unique needs.
There are three main types of SNPs: Dual Eligible SNPs (D-SNPs), Chronic Condition SNPs (C-SNPs), and Institutional SNPs (I-SNPs). Each type is designed to meet the needs of their specific populations. For example, D-SNPs cater to individuals who qualify for both Medicare and Medicaid, providing integrated care and additional benefits.
SNPs typically cover the same Medicare Part A and B benefits as other Medicare Advantage Plans, along with potential extra benefits. However, to remain eligible for an SNP, individuals must continue to meet specific criteria related to their health conditions.
Possible Benefits of Secure Horizons Medicare Advantage Plans

Secure Horizons Medicare Advantage Plans will likely provide extensive coverage choices that could address diverse healthcare needs. These plans might include additional benefits such as dental, vision, and hearing coverage, possibly making it easier for members to maintain their health without worrying about the cost. The vast provider network could potentially ensure availability for Medicare beneficiaries, so members can access the care they need wherever they are.
These potential benefits could make Secure Horizons plans an attractive option for those seeking comprehensive and affordable healthcare coverage.
Enrollment Process for Secure Horizons Medicare Advantage Plans
Individuals can evaluate and select their Medicare Advantage plans during the open enrollment period. This process is designed to be straightforward, ensuring that beneficiaries can find the plan that best meets their healthcare needs.
When to Enroll
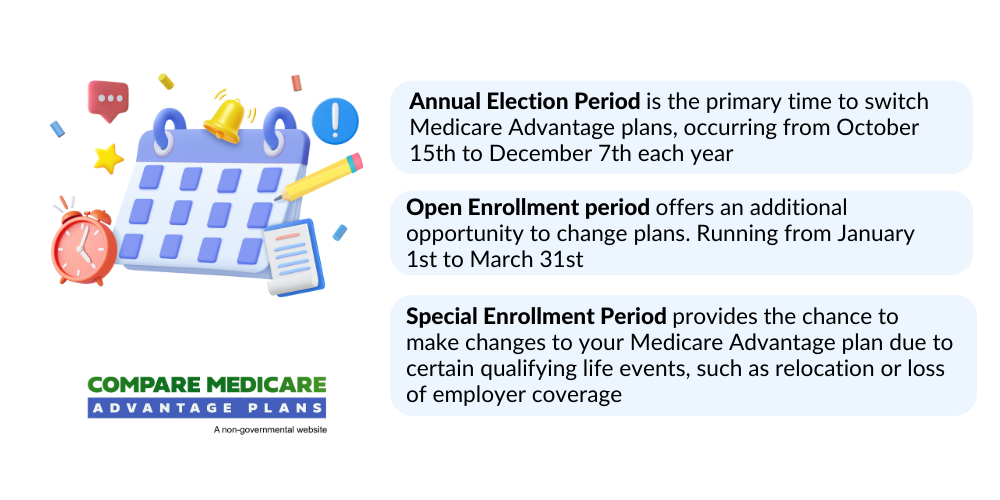
The annual enrollment period for Medicare Advantage plans occurs from October 15 to December 7. This is a critical time for beneficiaries to review their current coverage and make any necessary changes. The Initial Enrollment Period starts three months before you become eligible for Medicare and lasts until three months after. This period is particularly important for those who are newly eligible for Medicare, as it allows them to join any Medicare Advantage Plan.
During the Open Enrollment Period, from October 15 to December 7, you can switch or drop your Medicare Advantage Plan. Additionally, the Medicare Advantage Open Enrollment Period allows beneficiaries to change plans from January 1 to March 31 if they are already enrolled in a plan.
Special Enrollment Periods can occur under specific circumstances, such as moving or changes in current coverage.
Different Enrollment Periods
There are specific times, such as the annual enrollment period and special enrollment periods, when individuals can enroll or change their Medicare Advantage plans. Enrollees can also switch or change plans likely offering greater flexibility for those who may need to adjust their coverage more frequently.
The Annual Election Period remains from October 15 to December 7 for enrollees to join or change their Medicare Advantage plans. During the Open Enrollment Period from January 1 to March 31, individuals can switch from one Medicare Advantage plan to another or drop their plan.
OEP, AEP, Special Enrollment
The Open Enrollment Period (OEP) allows beneficiaries to make changes to their coverage after their initial enrollment. The Medicare Annual Enrollment Period (AEP) occurs from October 15 to December 7, allowing beneficiaries to modify their Medicare plans for the upcoming year. During this period, beneficiaries can switch between Medicare Advantage plans, return to Original Medicare, or adjust their current plan.
The Medicare Open Enrollment Period (OEP) is from January 1 to March 31, exclusively for individuals already enrolled in a Medicare Advantage plan, allowing limited changes. During this period, beneficiaries can make one plan change if they are currently enrolled in a Medicare Advantage plan, but multiple adjustments are not permitted.
Beneficiaries may qualify for a special enrollment period if they experience specific life events, such as losing employer coverage.
Possible Costs Associated with Secure Horizons Medicare Advantage Plans
Costs for Medicare Advantage plans might vary based on plan type and coverage options. Secure Horizons Medicare Advantage Plans will likely be designed to offer a cost-effective alternative to traditional Medicare, which may feature lower premiums and sometimes additional benefits.
Understanding these potential costs is crucial for beneficiaries to make informed decisions about their healthcare coverage.
Premiums and Co-Pays
Some Medicare Advantage plans may have lower monthly premiums, but other out-of-pocket expenses might still apply. Annual deductibles may differ, with some plans having separate deductibles for various medical services. Copayments are fixed fees that members pay for specific medical services, which could help budget expenses predictably. Coinsurance is typically a percentage of the total cost of a medical service that members are responsible for after their plan’s payment.
Some Secure Horizons plans might offer lower copays for primary care visits, likely promoting affordability for members. For chronic conditions, the average copays on C-SNP plans might be lower compared to standard Medicare Advantage plans. These plans will likely maintain stability in specialist and pharmacy copays.
Out-of-Pocket Maximums
Some Medicare Advantage plans may impose an out-of-pocket maximum that caps the total annual expenses members must pay for covered services. Once members reach their out-of-pocket maximum, they will not pay anything more for covered services for the remainder of the year. This potential feature could ensure that members are protected from excessive medical expenses, likely providing peace of mind.
Covered Services and Possible Benefits
Certain Medicare Advantage plans may offer lower out-of-pocket limits for certain services. The possible elimination of the Medicare donut hole could also benefit those needing prescription medications, likely making it easier to afford necessary treatments. Members of dual-eligible special needs plans (D-SNPs) may also be able to receive integrated care that coordinates both Medicaid and Medicare benefits.
How to Qualify for Secure Horizons Medicare Advantage Plans
Eligibility for Secure Horizons Medicare Advantage plans generally requires individuals to be enrolled in Medicare Parts A and B. Applicants must also reside in the service area of the Secure Horizons plan they wish to enroll in. Some plans may require individuals to have certain qualifying health conditions to enroll, particularly those designed for chronic care.
Enrollment periods are defined, and individuals must apply during these specific times to qualify for coverage. Certain plans cater to dual-eligible individuals, potentially providing additional benefits for those who qualify for both Medicare and Medicaid.
Comparing Secure Horizons Medicare Advantage Plans to Original Medicare
Secure Horizons Medicare Advantage Plans could provide a comprehensive alternative to Original Medicare, sometimes bundling additional benefits like vision and dental care. This could make them an attractive option for those seeking more extensive coverage.
Coverage Differences
Unlike Original Medicare, certain Secure Horizons plans might include integrated prescription drug coverage as part of their benefits. Some Medicare Advantage plans may also offer vision, dental, and hearing benefits.
Cost Comparisons
Some Secure Health Medicare Advantage plans might offer lower premiums and out-of-pocket costs for certain services. Special Needs Plans (SNPs) may also offer lower copays for frequently used benefits compared to standard Medicare plans. However, members still need to pay the standard Part B premium.
Emergencies and Referrals
Medicare Advantage plans may require referrals to see specialists, depending on the specific type of plan. However, in emergency situations, out-of-network providers are obligated to treat Medicare Advantage plan members. This ensures that members can receive the necessary care regardless of their location.
Traveling out of state could affect coverage under Medicare Advantage, depending on the plan’s network rules. Some Medicare Advantage plans may be designed for frequent travelers, likely allowing them to receive care from in-network providers nationwide. Additionally, emergency care is generally covered without requiring prior authorization from a primary care doctor.
Out-of-network emergency services will likely be covered at in-network rates by certain Medicare Advantage plans. Members should always seek emergency care if they believe their health is in danger, regardless of their plan’s rules.
Summary
Secure Horizons Medicare Advantage Plans for 2026 will likely offer a comprehensive and flexible alternative to Original Medicare. With a range of plan types, extensive coverage options, and potential benefits, these plans will likely be designed to meet the diverse needs of Medicare beneficiaries.
As we look towards the future, it’s clear that Secure Horizons will likely continue to innovate and expand its potential offerings, likely ensuring that members have access to the best possible care. Whether you’re managing chronic conditions or simply seeking a more comprehensive healthcare plan, Secure Horizons Medicare Advantage Plans could provide the stability and support needed to navigate your healthcare journey with confidence.
Frequently Asked Questions
→ When is the annual enrollment period for Medicare Advantage plans?
The annual enrollment period for Medicare Advantage plans is from October 15 to December 7. It’s important to mark these dates to ensure you can make any necessary changes to your coverage.
→ What are the main types of Secure Horizons Medicare Advantage Plans?
The main types of Secure Horizons Medicare Advantage Plans are Health Maintenance Organization (HMO) plans, Preferred Provider Organization (PPO) plans, and Special Needs Plans (SNPs). Each plan caters to different healthcare needs and preferences.
→ What additional benefits could Secure Horizons Medicare Advantage Plans 2026 offer?
Some Secure Horizons Medicare Advantage Plans may provide additional benefits like dental, vision, and hearing coverage, possibly enhancing your healthcare experience.
→ How could out-of-pocket maximums work in Medicare Advantage plans?
Once you reach your out-of-pocket maximum in a Medicare Advantage plan, you won’t have to pay anything more for covered services for the rest of the year. This potential feature could offer important financial protection against high medical costs.

ZRN Health & Financial Services, LLC, a Texas limited liability company



