Health Net Medicare Advantage Plans 2026
Wondering what Health Net Medicare Advantage Plans
Key Takeaways
- Health Net Medicare Advantage Plans offer a variety of options including HMO, PPO, and SNP plans, each with tailored benefits and coverage.
- Some plans may provide extensive services that could go beyond Original Medicare, such as dental, vision, and hearing coverage, with varying costs based on specific plans.
- Enrollment in Health Net plans is subject to contract renewal with Medicare, and members may access their benefits through a network of contracted providers for comprehensive care.
Compare Plans in One Step!
Enter Zip Code
Understanding Health Net Medicare Advantage Plans
Health Net will likely provide a range of Medicare Advantage plans, each tailored to meet the specific needs of different members. Some of these plans may go beyond traditional Medicare by potentially offering additional benefits such as dental, hearing, and vision coverage. Health Net’s Medicare Advantage plans will likely be designed to offer a comprehensive network of care and support for members, likely ensuring that all healthcare needs could be met efficiently.
Enrollment in Health Net plans is contingent upon the renewal of their contracts with Medicare, which means that availability may vary year to year. Members can use this website to manage their health and benefits effectively, making it easier for members to navigate their healthcare journey.
With options including HMO, PPO, and SNP plans, Health Net likely ensures that there is a suitable plan for everyone.
Types of Health Net Medicare Advantage Plans Available
Health Net offers a variety of Medicare Advantage plans tailored to meet diverse healthcare needs. These include Health Maintenance Organization (HMO) plans, Preferred Provider Organization (PPO) plans, and Special Needs Plans (SNPs). Each type has unique features and benefits designed to cater to different preferences and health requirements.
HMO Plans
Health Net’s HMO plans require members to select a primary care physician who coordinates all healthcare services, including referrals to specialists. This model ensures that members receive comprehensive and coordinated care, which can be crucial for managing chronic conditions and maintaining overall health. Members typically pay a fixed monthly premium, which might make it easier to predict healthcare costs.
These plans will likely offer extensive coverage that might include preventive care, emergency services, and hospitalization, among other plan benefits, likely making them a well-rounded option for many seniors.
Health Net also offers variations like Elect Open Access plans, which allow visits to PPO providers without referrals but with higher copays. Health Net’s HMO plans emphasize primary care coordination and predictable out-of-pocket costs, likely offering peace of mind and comprehensive care for members.
PPO Plans
Health Net’s PPO plans offer greater flexibility, allowing members to see any doctor, including out-of-network providers, often at a higher cost. Unlike HMO plans, PPO members do not need a primary care physician or referrals to see specialists, providing more freedom in choosing healthcare providers. This could be particularly advantageous for those who want more control over their healthcare choices.
Members of Health Net PPO plans can access a large network of medical providers, and in-network services typically result in lower out-of-pocket costs compared to out-of-network services. These plans provide comprehensive coverage, including a wide range of medical services, without the need for claims to be filed for in-network visits.
Health Net offers PPO plans at different metal levels such as platinum, gold, silver, and bronze, catering to various budget needs and preferences. This flexibility could make PPO plans an attractive option for those who prioritize choice and convenience in their healthcare.
Special Needs Plans (SNPs)
Special Needs Plans (SNPs) are designed for individuals with specific health conditions, offering tailored benefits and services. Health Net offers SNPs specifically for individuals with certain chronic conditions or those eligible for both Medicare and Medicaid. These plans provide additional benefits tailored to the unique health needs of their members, including specialized care coordination.
Eligibility for Health Net’s SNPs is determined based on specific criteria related to the member’s health status and financial situation. These plans focus on managing care for members with complex health issues, ensuring they have access to the necessary services. SNPs could be an excellent option for those who require more intensive and specialized care management.
By offering plans tailored to specific health needs, Health Net likely ensures that members could receive the appropriate care and services to manage their conditions effectively.
Overview of Health Net Medicare Advantage
Health Net will likely provide a comprehensive range of Medicare Advantage plans that could integrate additional benefits beyond standard Medicare. These offerings include HMO, HMO SNP, and PPO plans, each designed to cater to different healthcare needs. Health Net ensures that their Medicare Advantage plans could provide a broad network of care and support for members.
Enrollment in Health Net Medicare Advantage plans is subject to contract renewal, which might impact plan availability. As an affiliate of Centene Corporation, Health Net likely benefits from extensive support and resources, possibly enhancing the overall member experience. This affiliation could ensure that members have access to high-quality care and a wide range of benefits.
Covered Services and Potential Benefits

Health Net Medicare Advantage Plans will likely provide coverage for a variety of medical services, including preventive care, hospitalization, and skilled nursing facility services. Members may also have access to additional benefits such as vision and dental care, which are not typically included in Original Medicare.
Prescription drug coverage may also be included in certain plans, possibly ensuring that members could have access to necessary medications. These comprehensive benefits could make some Health Net plans a robust option for managing overall health.
Possible Benefits of Health Net Medicare Advantage Plans
Some Health Net Medicare Advantage Plans might offer additional coverage that could go beyond Original Medicare. This might include dental, vision, and hearing care, which could significantly enhance a member’s quality of life. These potential features could make Health Net Medicare Advantage Plans a comprehensive and convenient option for seniors.
Enrollment Process for Health Net Medicare Advantage Plans
The enrollment process for Health Net Medicare Advantage plans typically starts with determining eligibility based on Medicare guidelines. Individuals can enroll by using this website or by calling one of our licensed agents at 1-833-641-4938 (TTY 711), Mon-Fri 8 am-9 pm EST.
Knowing when and how to enroll may help maximize the benefits of these plans. Whether you are enrolling for the first time or switching plans, knowing the different enrollment periods can help you make an informed decision.
When to Enroll
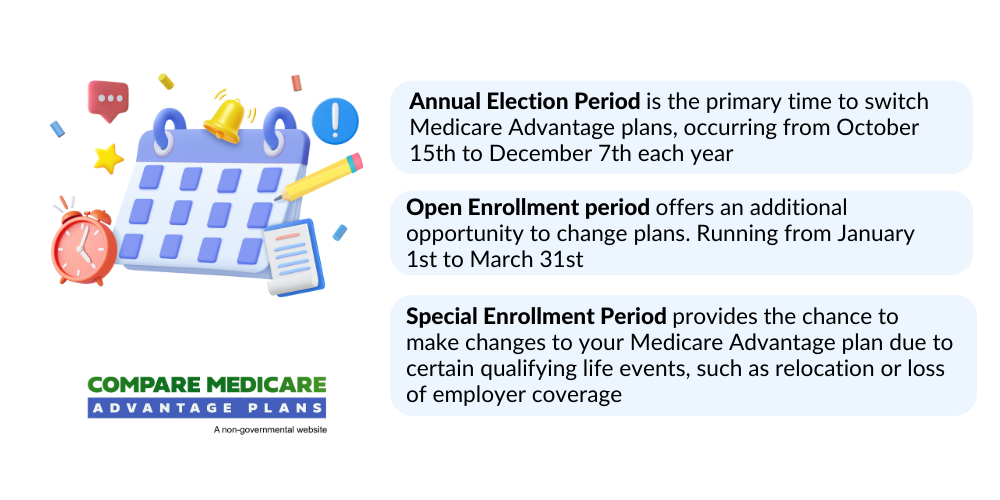
Individuals can enroll in Health Net Medicare Advantage plans during their initial enrollment period, which begins three months before they turn 65. This period includes the birthday month and lasts for three months afterward. Enrollment can also occur during the Annual Election Period from October 15 to December 7 each year.
Special Enrollment Periods are available for those who experience certain life events, such as moving or losing other health coverage. These periods provide flexibility for individuals to enroll in or change their Medicare Advantage plans outside of the standard enrollment windows.
Different enrollment periods
There are specific times throughout the year when individuals can enroll in or change their Medicare Advantage plans, known as enrollment periods. The Annual Enrollment Period (AEP) runs from October 15 to December 7, allowing beneficiaries to make changes to their plans.
The Open Enrollment Period (OEP) occurs from January 1 to March 31, during which enrollees can switch plans or revert to Original Medicare. Special Enrollment Periods (SEPs) allow for plan changes due to qualifying life events, such as moving or losing other coverage.
OEP, AEP, Special Enrollment
The Open Enrollment Period (OEP) allows beneficiaries to change their Medicare Advantage plans once a year, providing an opportunity to adjust coverage based on changing health needs. The Annual Election Period (AEP) occurs from October 15 to December 7, enabling new enrollments and changes to existing plans.
Special Enrollment Periods (SEPs) allow members to change plans due to qualifying life events, such as moving or losing other coverage. These periods are essential for making informed healthcare coverage decisions.
Possible Costs Associated with Health Net Medicare Advantage Plans
Health Net Medicare Advantage plans will likely have various costs such as premiums, co-pays, and deductibles, which might vary based on specific plan choices. These costs will likely be crucial for budgeting and planning healthcare expenses.
These costs may be influenced by factors such as the type of plan chosen, the level of coverage, and whether services are received in-network or out-of-network.
Premiums and Co-Pays
Some Health Net Medicare Advantage plans might require monthly premiums in addition to co-pays for certain services, depending on their plan type. These costs may vary significantly, with some plans offering low premiums but higher co-pays for services.
Balancing premiums and co-pays could be key to selecting a plan that fits your budget and healthcare needs. It’s important to review the possible costs associated with each plan to make an informed decision.
Out-of-Pocket Maximums
Certain Health Net Medicare Advantage plans might set out-of-pocket maximum limits, possibly providing a cap on how much members could pay for covered services in a plan year.
Once the out-of-pocket maximum is met, no further cost-sharing is required for essential health benefits for the rest of the year. This cap could help protect members from excessive healthcare costs and may also provide financial peace of mind.
Covered Services and Potential Benefits
Health Net Medicare Advantage plans will likely provide a comprehensive range of services, likely ensuring that members could receive the care they need. These plans will likely cover hospital stays, outpatient care, preventive services, and sometimes prescription drug coverage. Additionally, members could potentially benefit from dental, vision, and hearing services, which are not typically covered by Original Medicare.
Emergency services are covered under all Health Net Medicare Advantage plans, regardless of provider network status. Members will likely have access to a network of healthcare providers, possibly ensuring a wide range of services to meet their medical needs.
How to Qualify for Health Net Medicare Advantage Plans
To qualify for Health Net Medicare Advantage plans, individuals must be enrolled in Medicare Parts A and B. Applicants must also reside within the Health Net service area to be eligible for these plans. Certain plans might exclude individuals with end-stage renal disease (ESRD) unless specific criteria are met.
During the application process, potential enrollees may need to provide personal information, including health history and current medications. Enrollment is typically available during specific periods such as the Annual Enrollment Period (AEP).
Meeting these clinical criteria and medical necessity criteria is essential for eligibility and successful enrollment.
Contracted Network and Access to Care
Health Net Medicare Advantage plans will likely utilize a network of contracted providers, possibly ensuring that members receive the highest level of coverage when using in-network services. Members may see out-of-network providers, but additional costs may apply. Emergency services are covered regardless of whether the provider is in-network or out-of-network.
Access to care might vary based on geographic location, with different plans offering different networks. Health Net could connect members to a broad network of hospitals and health care providers. Knowing the difference between an in network provider and out-of-network providers helps manage healthcare costs effectively.
Comparing Health Net Medicare Advantage Plans to Original Medicare
Some Health Net Medicare Advantage plans might offer additional benefits not covered by Original Medicare, such as routine dental, hearing, and vision care. Certain plans could potentially provide a more comprehensive approach to healthcare, possibly ensuring that members could receive the services they need to maintain their health.
Coverage Differences
Original Medicare provides standardized coverage for hospital and medical services but lacks additional benefits like dental and vision care. Certain Health Net Medicare Advantage plans might include these extra services, possibly making them a more attractive option for many beneficiaries.
While Original Medicare has nationwide acceptance, Health Net plans will likely operate within specific regional networks, which could impact access to care. However, some Health Net plans may include integrated care management services, which could enhance care coordination compared to Original Medicare.
Cost Comparisons
The potential costs associated with Health Net Medicare Advantage plans might include premiums, deductibles, and out-of-pocket maximums may vary significantly among plans. These cost variations will likely make it essential for beneficiaries to carefully compare plans to find the best fit for their needs and budget.
Emergencies and Referrals

In emergencies, members do not need a referral to receive care, ensuring immediate access to necessary medical services. Health Net Medicare Advantage PPO members can seek care from out-of-network providers without needing a referral, offering greater flexibility in emergency situations.
For non-emergency services, prior authorization may be required, meaning a member’s primary care physician must approve certain types of care before they are received.
Understanding these regulatory requirements and evidence-based guidelines is crucial for managing healthcare effectively.
Summary
Health Net Medicare Advantage Plans
By understanding the potential costs, covered services, and enrollment periods, beneficiaries can make informed decisions about their healthcare. Whether you are new to Medicare or considering a switch, Health Net Medicare Advantage Plans will likely provide a valuable option for managing your health
Frequently Asked Questions
→ What types of Medicare Advantage plans does Health Net offer?
Health Net provides HMO, PPO, and Special Needs Plans (SNPs) to meet diverse healthcare requirements. Each plan is designed to accommodate specific needs, ensuring suitable coverage options for members.
→ What additional benefits could Health Net Medicare Advantage Plans 2026 provide?
Some Health Net Medicare Advantage Plans may provide additional benefits such as dental, vision, and hearing care, possibly enhancing overall healthcare access and support.
→ When can I enroll in a Health Net Medicare Advantage Plan?
You can enroll in a Health Net Medicare Advantage Plan during your Initial Enrollment Period, the Annual Election Period from October 15 to December 7, or during Special Enrollment Periods if you qualify due to specific life events.
→ Are there out-of-pocket maximums with Health Net Medicare Advantage Plans 2026 ?
Unfortunately, the plan details

ZRN Health & Financial Services, LLC, a Texas limited liability company




