Aetna Medicare Advantage Plans Georgia 2026
Are you considering Aetna Medicare Advantage Plans in Georgia
Key Takeaways
- Aetna Medicare Advantage plans in Georgia will likely offer comprehensive healthcare services tailored to the needs of residents, and may include additional benefits, such as dental, vision, and hearing coverage.
- Available plans include various options such as HMO, PPO, and Special Needs Plans (SNPs), each designed to cater to different healthcare preferences and requirements.
- Certain Aetna Medicare Advantage plans might integrate prescription drug coverage, which could offer low premiums, possibly making them a compelling choice compared to Original Medicare.
Compare Plans in One Step!
Enter Zip Code
Overview of Aetna Medicare Advantage Plans in Georgia

Aetna will likely offer a variety of Medicare Advantage plans tailored specifically for Georgia residents, focusing on affordability and comprehensive health management. These plans are designed to provide a more holistic approach to healthcare, addressing not only medical needs but may also incorporate additional benefits such as dental, vision, and hearing services.
This could potentially ensure that members can access a wide range of healthcare services under one plan, enhancing their overall well-being.
The possible benefits and availability of these plans may vary by service area within Georgia. Reviewing plan details carefully could help ensure they meet your healthcare needs.
Types of Aetna Medicare Advantage Plans
Aetna’s Medicare Advantage plans in Georgia will likely encompass various types, each designed to cater to different healthcare needs and preferences. These include Health Maintenance Organization (HMO) plans, Preferred Provider Organization (PPO) plans, and Special Needs Plans (SNPs). Each type offers unique features and benefits, so understanding these differences helps in choosing the most suitable plan for your situation.
The HMO plans typically require members to choose a primary care provider and get referrals for specialist visits, offering coordinated healthcare through a network of providers. PPO plans, on the other hand, provide greater flexibility, allowing members to see any doctor or specialist without a referral.
Special Needs Plans (SNPs) are tailored for individuals with specific health needs, such as those eligible for both Medicare and Medicaid. Let’s delve deeper into each of these plan types.

HMO Plans
Health Maintenance Organization (HMO) plans are structured to provide coordinated healthcare through a network of providers. Members are required to select a primary care provider (PCP), who becomes the central point of contact for all healthcare needs. This PCP coordinates care and provides referrals to specialists, streamlining and managing medical services effectively.
While this system can lead to more organized and efficient care, it also means that out-of-network services are typically not covered, except in emergencies. HMO plans often come with additional benefits like dental and vision care, enhancing overall healthcare access.
These benefits could make HMO plans a popular choice for those who prefer having a single point of contact for their healthcare needs and are comfortable with the network restrictions. For those who value coordinated care and don’t mind the referral system, an HMO plan might be the right fit.
PPO Plans
Preferred Provider Organization (PPO) plans offer more flexibility compared to HMO plans. Members can see any doctor or specialist without needing a referral, making it easier to access healthcare services. This flexibility could be particularly beneficial for those who prefer having the freedom to choose their healthcare providers. Additionally, PPO plans allow members to receive care from both in-network and out-of-network providers, although using out-of-network services typically incurs higher costs.
Despite the higher out-of-pocket costs for out-of-network care, many find the flexibility of PPO plans appealing. These plans are suitable for individuals who value the ability to see specialists without referrals and are willing to pay more for out-of-network services. For those who prioritize flexibility and choice in healthcare providers, a PPO plan might be the best option.
Special Needs Plans (SNPs)
Special Needs Plans (SNPs) are specifically designed for individuals with particular health needs, such as those eligible for both Medicare and Medicaid or those with chronic conditions. These plans provide tailored benefits to address the unique health challenges faced by their members.
For example, Dual-Eligible Special Needs Plans (D-SNPs) cater to individuals who qualify for both Medicare and Medicaid, offering integrated benefits that cover a wide range of services. Similarly, Chronic Condition Special Needs Plans (C-SNPs) are available for individuals with specific chronic conditions, providing specialized care and benefits.
Enrollment in these plans requires checking availability in the member’s location and completing the necessary paperwork. For those with specific health needs requiring specialized care, an SNP might be the ideal choice.
Prescription Drug Coverage
Some of Aetna’s Medicare Advantage plans in Georgia may include integrated prescription drug coverage. This possible integration could simplify access by potentially combining medical coverage and prescription benefits under one plan. The prescription drug coverage is categorized into five tiers, with Tier 1 being the most affordable and Tier 5 the most expensive.
The formulary details which drugs may be covered and any associated requirements like prior authorization or quantity limits. Certain drugs may have stipulations, such as requiring prior approval or having limits on the quantity that can be dispensed. This could help ensure that members have access to necessary medications while maintaining cost-effectiveness.
Comparing Costs: Aetna Medicare Advantage vs. Original Medicare
Medicare Advantage plans will likely have varying premiums, deductibles, and copayments, which might make them more cost-effective than Original Medicare, depending on individual health needs. One of the possible advantages of Medicare Advantage plans may be the annual maximum out-of-pocket limit. This could provide a financial safety net that Original Medicare does not offer.
Costs for Medicare Advantage plans may vary widely based on the specific plan chosen, possibly affecting overall out-of-pocket expenses compared to Original Medicare. For most doctor visits, Medicare Advantage will likely require a copayment, whereas Original Medicare users may only have to pay a coinsurance of up to 20% for services.
Evaluating your healthcare needs and financial situation is crucial when choosing between Medicare Advantage and Original Medicare coverage and Original Medicare.
Potential Benefits of Aetna Medicare Advantage Plans

Certain Aetna Medicare Advantage plans may offer a range of benefits designed to address overall health, including services beyond what Original Medicare covers. Some Aetna plans may offer additional perks such as dental, hearing, and vision coverage. These plans may also include dental coverage for checkups, cleanings, and X-rays, possibly making them an attractive option for those seeking a comprehensive medicare plan.
Vision benefits might include annual eye exams and coverage for glasses or contact lenses while hearing coverage could feature annual exams and assistance with hearing aids and fittings.
Types of Enrollment and When They Occur
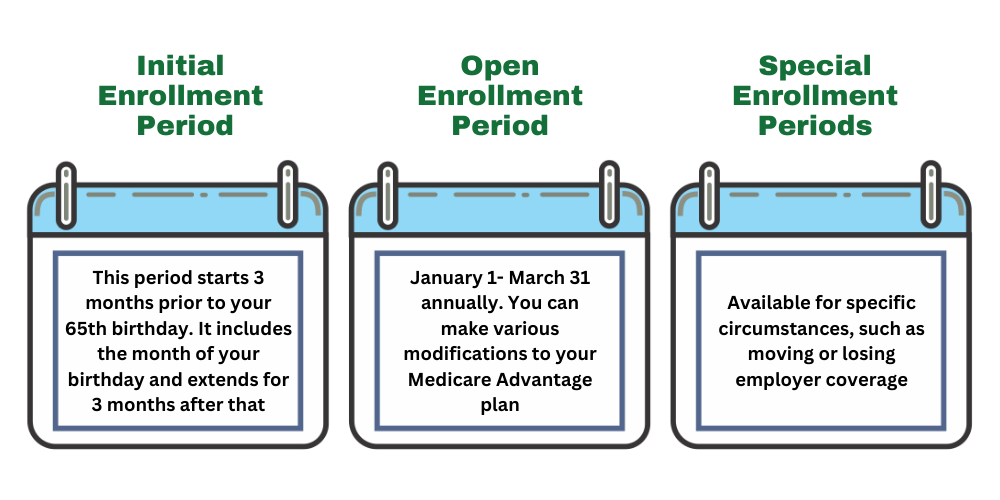
When considering the potential Aetna Medicare Advantage plans in Georgia, understanding the different enrollment periods is crucial to ensure you can sign up for or make changes to your plan at the appropriate time. Here are the key types of enrollment periods:
Initial Enrollment Period (IEP)
The Initial Enrollment Period is a seven-month window that begins three months before you turn 65, includes your birth month, and extends three months after. During this time, you can enroll in a Medicare Advantage plan for the first time. It’s an excellent opportunity to explore Aetna’s potential offerings, such as medical coverage, prescription drug coverage, and additional benefits like dental and vision services.
Annual Enrollment Period (AEP)
The Annual Enrollment Period runs from October 15 to December 7 each year. This period allows you to make changes to your existing Medicare Advantage plan or switch from Original Medicare to a Medicare Advantage plan, such as those offered by Aetna. During AEP, you can also join or change your prescription drug plan to better suit your healthcare needs.
Special Enrollment Period (SEP)
Special Enrollment Periods are triggered by specific life events, such as moving out of your plan’s service area, losing other health coverage, or qualifying for Medicaid. These periods allow you to enroll in or switch Medicare Advantage plans outside the standard enrollment windows. If you experience a qualifying event, it’s vital to act promptly to ensure continuous coverage.
Medicare Advantage Open Enrollment Period
From January 1 to March 31, the Medicare Advantage Open Enrollment Period allows those already enrolled in a Medicare Advantage plan to make a one-time change. You can switch to another Medicare Advantage plan or return to Original Medicare. This period is particularly beneficial if you find your current plan doesn’t meet your expectations or healthcare needs.
Understanding these enrollment periods likely ensures you can take full advantage of the possible benefits offered by Aetna Medicare Advantage plans, aligning your healthcare coverage with your personal needs and preferences.
Access to Care and Network
Aetna’s HMO plans require members to use a network of doctors and hospitals, which may necessitate a referral from a primary care provider for specialist visits. This network-based approach will likely ensure coordinated care and effective management of healthcare services. Using preferred network pharmacies may also lead to lower cost shares for Aetna Medicare members.
Emergency and Referral Policies
In HMO plans, receiving care outside of the network might incur higher costs, except in emergencies. However, during declared public health emergencies or disasters, some Aetna Medicare Advantage plans may temporarily adjust out-of-network costs to match in-network rates. This policy could potentially ensure that members are not financially burdened during critical times when access to in-network providers might be limited.
Aetna may also waive referral requirements during certain emergencies and might implement immediate changes that benefit members without the standard 30-day notice during emergencies. These policies protect members and ensure they receive necessary care without undue financial strain.
Star Ratings and Plan Evaluations

Every year, Medicare evaluates plans based on a 5-star rating system, influencing Aetna’s contract renewal process. These star ratings could impact enrollment eligibility and guide members in choosing the best plans during enrollment periods. A plan with a high star rating indicates better performance in areas such as customer service, member satisfaction, and overall health management.
The results of the star ratings affect Aetna’s contract renewal process and influence member choices during enrollment periods. This system ensures plans consistently improve and meet member needs, providing a reliable indicator of plan quality and performance.
Contract Renewal and Changes
Aetna Medicare plans will likely be subject to annual medicare contract renewal, which could affect enrollment and benefits. Enrollment in Aetna Medicare Advantage plans is contingent upon the renewal of contracts with Medicare. This annual review process ensures that the plans continue to meet Medicare’s standards and provide the necessary benefits to their members.
As a result, Aetna Medicare Advantage members may need to review their coverage annually due to potential changes in plan benefits. Staying informed about these changes could potentially ensure the selected plan continues to meet individual healthcare needs effectively.
Summary
Navigating the world of Medicare may be complex, but understanding the specifics of Aetna Medicare Advantage Plans in Georgia could help in making informed decisions. Some plans might offer a variety of benefits that could go beyond Original Medicare, such as dental, vision, and hearing services. The different types of plans—HMO, PPO, and SNP—cater to diverse healthcare needs, providing flexibility and tailored benefits.
Comparing the potential costs and benefits between Aetna Medicare Advantage Plans and Original Medicare could reveal the potential for more comprehensive coverage and financial protection. With the possibility of having integrated prescription drug coverage and a structured enrollment process, these plans have been designed to make healthcare accessible and manageable.
As you consider your options, remember that the star ratings and contract renewal processes ensure that these plans maintain high standards of care. Ultimately, Aetna Medicare Advantage Plans could offer a robust solution for managing your healthcare needs in Georgia.
Frequently Asked Questions
→ What types of Aetna Medicare Advantage Plans are available in Georgia?
Aetna Medicare Advantage Plans available in Georgia include HMO, PPO, and Special Needs Plans (SNPs), ensuring a range of options for varying healthcare needs.
→ Do Aetna Medicare Advantage Plans include prescription drug coverage?
Yes, some Aetna Medicare Advantage Plans might integrate prescription drug coverage, possibly offering access to a wide range of medications.
→ How do Aetna Medicare Advantage Plans compare to Original Medicare in terms of costs?
Certain Aetna Medicare Advantage Plans may be more cost-effective than Original Medicare due to varying premiums, deductibles, and copayments, along with the possible benefit of an annual maximum out-of-pocket limit that Original Medicare lacks. This financial safety net could lead to overall savings for beneficiaries.
→ What additional benefits could Aetna Medicare Advantage Plans offer?
Some Aetna Medicare Advantage Plans may provide additional benefits such as dental, vision, and hearing services. These potential features could enhance overall health and wellness for members.
→ What is the enrollment process for Aetna Medicare Advantage Plans?
To enroll in an Aetna Medicare Advantage Plan, you must first be enrolled in Original Medicare (Parts A and B). You can complete your enrollment by calling a licensed agent at 833-641-4938.

ZRN Health & Financial Services, LLC, a Texas limited liability company
Russell Noga is the CEO of ZRN Health & Financial Services, and head content editor of several Medicare insurance online publications. He has over 15 years of experience as a licensed Medicare insurance broker helping Medicare beneficiaries learn about Medicare, Medicare Advantage Plans, Medigap insurance, and Medicare Part D prescription drug plans.