Medicare Advantage Plans Tennessee 2026
Looking for the best Medicare Advantage plan in Tennessee
Key Takeaways
- Over 1.4 million Tennesseans are enrolled in Medicare, with nearly half opting for Medicare Advantage plans due to their comprehensive coverage and potential benefits.
- Medicare Advantage plans in Tennessee might include various types, such as HMO, PPO, and SNPs, each offering unique features tailored to beneficiaries’ healthcare needs.
- Enrollment in Medicare Advantage plans is accessible, with defined periods for Initial, Annual, and Special Enrollment, and some plans may help limit out-of-pocket costs for certain services.
Compare Plans in One Step!
Enter Zip Code
Overview of Medicare Advantage Plans in Tennessee

Over 1.4 million Tennesseans are enrolled in Medicare since 2023, accounting for about approximately 20% of the state’s population. Among these beneficiaries, nearly half opted for Medicare Advantage plans, reflecting their growing popularity. Some plans could offer a single solution for various healthcare needs, possibly simplifying access to care for enrollees.
Medicare Advantage plans allow beneficiaries to receive their Medicare benefits through private insurance companies approved by Medicare. This setup may also include additional benefits not covered by Original Medicare, possibly making them an attractive option for many.
What Are Medicare Advantage Plans?
Medicare Advantage plans are private insurance plans that could serve as an alternative to Original Medicare. These plans typically bundle hospital care, medical services, and sometimes includes additional benefits like dental, vision, and prescription drug coverage. This comprehensive approach could make these plans a preferred choice for many Medicare beneficiaries.
Certain Medicare Advantage plans may also include integrated prescription drug coverage. This potential combination of services could enhance the overall healthcare experience for beneficiaries, possibly providing a more robust selection of benefits compared to Original Medicare.
Differences Between Medicare Advantage and Original Medicare
Some Medicare Advantage plans may include additional benefits that Original Medicare might not cover, such as vision, dental, and hearing coverage. These potential benefits could be particularly beneficial for those who require comprehensive healthcare services. However, members should review their plan’s drug formulary to ensure that the medications they need are covered.
Another difference might be the network of providers. Medicare Advantage HMO plans typically require enrollees to use in-network doctors and hospitals, which can impact access to care. Conversely, receiving healthcare outside the Medicare Advantage HMO network may result in higher out-of-pocket costs or uncovered services.
Possible Benefits of Choosing Medicare Advantage Plans in Tennessee
Some Medicare Advantage plans in Tennessee may be highly favored for their comprehensive nature, which may bundle hospital, medical, and additional services into a single plan. This could make them a convenient and attractive option for many beneficiaries. The potential ability to receive extra services such as dental, vision, and hearing benefits might further enhance their appeal.
Choosing a Medicare Advantage plan in Tennessee could also lead to potential cost savings. Various insurance companies might offer these plans, with some being highly rated for member experience and overall service quality. This could potentially ensure that beneficiaries receive high-quality care and support, possibly making these plans a top choice for many.
Comprehensive Coverage
Some Medicare Advantage plans in Tennessee may combine the benefits of Original Medicare with additional services, possibly providing comprehensive healthcare coverage under a single plan. This might include services such as vision and dental care, which are not typically covered by Original Medicare. This streamlined access to care could potentially ensure that member;s healthcare needs are met efficiently and effectively.
Types of Medicare Advantage Plans Available in Tennessee
Tennessee will likely offer a variety of Medicare Advantage plans to cater to the diverse needs of its residents. These include Health Maintenance Organizations (HMO), Preferred Provider Organizations (PPO), and Special Needs Plans (SNPs). Each type of plan has unique features and benefits, allowing beneficiaries to choose the one that best suits their healthcare needs.
Providers like Humana and UnitedHealthcare may offer multiple Medicare Advantage options. These options could potentially ensure that beneficiaries can find a plan that fits their specific healthcare requirements.
Health Maintenance Organization (HMO) Plans
Medicare Advantage HMO plans generally require members to use a specific network of providers, which can impact access to healthcare services. Members typically receive healthcare exclusively from in-network providers, except in emergencies. This ensures coordinated care and can lead to lower out-of-pocket costs.
However, HMO plans often require referrals to see specialists, which can be a consideration for those who frequently need specialized care. Despite this, the structured care approach of HMO plans can be beneficial for managing overall healthcare.
Preferred Provider Organization (PPO) Plans
PPO plans offer greater flexibility compared to HMO plans, allowing members to see a variety of healthcare providers. Members can choose to see out-of-network providers, although this comes with higher costs compared to in-network services. This flexibility can be particularly beneficial for those who travel frequently or have preferred providers outside the network.
PPO plans do not typically require referrals to see specialists, making it easier for beneficiaries to access the care they need when they need it.
Special Needs Plans (SNPs)
Special Needs Plans (SNPs) are designed specifically for individuals with chronic conditions, offering specialized healthcare benefits tailored to their needs. These plans provide targeted care management and coordination, ensuring that beneficiaries receive the appropriate care for their specific health conditions.
SNPs can be a valuable option for those with chronic illnesses, providing access to specialized services and support that may not be available through other Medicare Advantage plans.
Top-Rated Medicare Advantage Providers in Tennessee

Enrollment in Medicare Advantage plans in Tennessee has been on the rise, with an approximate 7% increase between 2021 and 2022. This growth reflects the high satisfaction and trust beneficiaries have in these plans. Top providers in Tennessee are evaluated based on member ratings, coverage options, and overall satisfaction.
Based on data form previous years, some of the top providers are BlueCross BlueShield of Tennessee, Humana, and UnitedHealthcare. These companies will likely offer a range of medical insurance plans tailored to meet the diverse needs of beneficiaries, ensuring high-quality care and support.
BlueCross BlueShield of Tennessee
BlueCross BlueShield of Tennessee will likely provide a variety of Medicare Advantage plans designed to meet the specific needs of its members. Some plans may include additional benefits such as vision and dental care. Customer feedback likely indicates that members appreciate the ease of access to healthcare services and the support provided by BlueCross BlueShield.
Overall, BlueCross BlueShield has received positive reviews for its responsive customer service and satisfactory claim handling. This could make them a reliable choice for many Tennessee residents.
Humana
Humana will likely offer a variety of Medicare Advantage plans that have been known for their quality and member satisfaction ratings. Some plans might provide comprehensive coverage, including hospital stays, and doctor visits.
Humana’s commitment to high-quality care and member satisfaction likely makes it a top choice for many beneficiaries in Tennessee.
UnitedHealthcare
In recent years, UnitedHealthcare has held a high average star rating of approximately 4.17, reflecting strong performance in customer satisfaction. Their Medicare Advantage plans will likely be recognized for their extensive provider networks, possibly offering members a broad choice of healthcare providers.
With a variety of plan options tailored to meet different healthcare needs, UnitedHealthcare could be a reliable and popular choice for many Tennessee residents.
How to Enroll in a Medicare Advantage Plan in Tennessee
Enrolling in a Medicare Advantage plan in Tennessee is a simple process. Eligibility is based on age, disability, or specific health conditions, and individuals must live within the geographic service area of the plan they wish to enroll in. The Tennessee State Health Insurance Assistance Program offers help with questions regarding Medicare eligibility and enrollment.
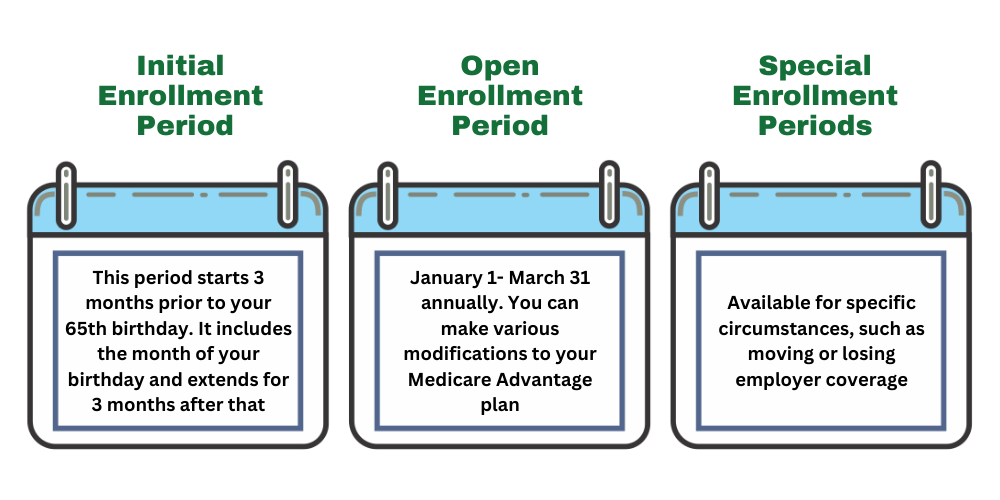
There are three primary enrollment periods: the Initial Enrollment Period, the Annual Enrollment Period, and Special Enrollment Period. Each of these periods provides an opportunity for beneficiaries to enroll in or change their Medicare Advantage plans.
Initial Enrollment Period
The Initial Enrollment Period lasts seven months, starting three months before the individual turns 65. This enrollment period begins on the first day of the month in which the individual turns 65.
During this time, new Medicare beneficiaries can enroll in Medicare Advantage plans, ensuring they have coverage as soon as they are eligible.
Annual Enrollment Period
The Annual Enrollment Period for Medicare occurs from October 15 to December 7 each year. During this period, beneficiaries can make changes to their Medicare coverage, including their Part D plans.
Changes made during the Annual Enrollment Period take effect on January 1 of the following year.
Special Enrollment Period
A Special Enrollment Period (SEP) in Medicare Advantage is a period outside the Initial and Annual Enrollment periods when beneficiaries can make changes to their plans. SEPs can be triggered by specific life events, such as moving to a new area or losing other health coverage.
Beneficiaries can find guidance for Special Enrollment Periods by contacting one of our licensed agents at 1-833-641-4938 (TTY 711), Mon-Fri 8 am-9 pm EST.
Understanding Medicare Advantage Costs
Understanding the potential costs associated with Medicare Advantage plans will likely be crucial for budgeting and avoiding unexpected expenses. These costs might include monthly premiums, deductibles, copayments, and out-of-pocket maximums.
Some Medicare Advantage plans might offer out-of-pocket costs with maximum spending caps, which Original Medicare does not provide.
Deductibles and Copayments
A deductible in the context of Medicare Advantage plans is an amount paid out of pocket before the plan covers services. These plans might include copayments, coinsurance, and deductibles, which could affect the overall out-of-pocket costs for beneficiaries.
Understanding these potential costs could help beneficiaries budget for their healthcare services and possibly avoid unexpected expenses.
Out-of-Pocket Maximums
Certain Medicare Advantage plans may offer out-of-pocket maximums that could limit the total annual amount beneficiaries must pay for covered services. This cap might encompass copayments, coinsurance, and deductibles. It will likely apply specifically to services covered by Medicare.
These out-of-pocket maximums could help beneficiaries budget their healthcare expenses by potential capping annual spending, possibly providing financial peace of mind.
Resources for Tennessee Medicare Beneficiaries
Tennessee will likely offer a wealth of resources to help Medicare beneficiaries navigate their healthcare options. The Tennessee Commission on Aging and Disability serves as a valuable resource, providing information and assistance to senior residents. Additionally, the Tennessee State Health Insurance Assistance Program (SHIP) offers guidance regarding Medicare eligibility and enrollment, ensuring beneficiaries understand their options.
The Tennessee Department of Commerce and Insurance offers assistance for consumers. They provide guidance on various insurance-related questions. These resources are essential for Tennessee residents, helping them make informed decisions about their Medicare Advantage plans.
Summary
Choosing the right Medicare Advantage plan in Tennessee
Some of the top0rrated providers like BlueCross BlueShield of Tennessee, Humana, and UnitedHealthcare may offer a range of plans tailored to meet diverse healthcare requirements. Understanding the enrollment periods and potential costs associated with these plans could be crucial for making an informed decision. Utilize the available resources in Tennessee to guide you through the process and ensure you choose the best plan for your needs.
Frequently Asked Questions
→ What are Medicare Advantage plans?
Medicare Advantage plans are privately offered insurance options that could serve as an alternative to Original Medicare and might include extra benefits like prescription drug coverage, vision, dental, and hearing coverage. This could potentially give you more comprehensive coverage tailored to your healthcare needs.
→ How do Medicare Advantage plans differ from Original Medicare?
Some Medicare Advantage plans might provide additional benefits like vision, dental, and dental coverage that Original Medicare does not offer. However, some plans may also require using in-network providers, which may limit your access to care. This distinction is essential when considering your healthcare options.
→ What types of Medicare Advantage plans are available in Tennessee?
Tennessee will likely provides several types of Medicare Advantage plans, such as Health Maintenance Organizations (HMO), Preferred Provider Organizations (PPO), and Special Needs Plans (SNPs). Choosing the right plan is essential for meeting your healthcare needs.
→ How can I enroll in a Medicare Advantage plan in Tennessee?
To enroll in a Medicare Advantage plan in Tennessee, you can do so during the Initial Enrollment Period, Annual Enrollment Period, or Special Enrollment Periods, provided you meet eligibility criteria based on age, disability, or health conditions, and reside within the plan’s service area.
→ What are the potential costs associated with Medicare Advantage plans?
Some Medicare Advantage plans might involve monthly premiums, deductibles, copayments, and out-of-pocket maximums, which could help govern annual spending.

ZRN Health & Financial Services, LLC, a Texas limited liability company