UnitedHealthcare Medicare Advantage Plans South Dakota 2026
Looking into the potential UnitedHealthcare Medicare Advantage Plans for South Dakota in 2026? This article highlights the potential benefits, coverage options, and the enrollment process. Find out what you could expect from your Medicare plan next year.
Key Takeaways
- Some UnitedHealthcare Medicare Advantage Plans in South Dakota might offer additional benefits, such as dental, vision, and hearing aids, tailored to member needs.
- The enrollment process is straightforward with specific periods for initial signup, annual changes, and exceptions.
- Members will likely have access to various healthcare services and support resources, possibly ensuring they can choose the best plan for their healthcare needs.
Compare Plans in One Step!
Enter Zip Code
Overview of UnitedHealthcare Medicare Advantage Plans in South Dakota
UnitedHealthcare Medicare Advantage Plans in South Dakota will likely aim to provide a diverse range of plans that could be tailored to the unique healthcare needs of enrollees. These plans could potentially ensure members receive comprehensive coverage that aligns with their specific health requirements. Whether you need regular medical checkups or specialist care, these plans could offer a holistic approach to healthcare.
The potentila benefits and features of these plans may vary depending on the specific plan and local area. This means that while some benefits are universally available, others might be unique to certain regions. Enrollees should carefully review the plan details to fully understand the potential benefits and ensure they match their healthcare needs.
Possible Benefits of UnitedHealthcare Medicare Advantage Plans

UnitedHealthcare Medicare Advantage Plans are designed to cover essential medical services, possibly ensuring that members receive the care they need without unnecessary financial burdens. Coverage typically includes hospital stays, specialist visits, and routine checkups, creating a solid foundation for healthcare needs.
Additionally, some plans may also offer coverage for dental care, which may include routine exams, cleanings, and certain procedures. Vision care benefits may also be included, possibly offering annual eye exams and allowances for lenses or frames, although the specifics might vary based on the plan.
Hearing aids could be another potential benefit, which may be covered when obtained through UnitedHealthcare’s designated network providers. These potential comprehensive health benefits could ensure that members have access to essential care across various medical needs.
Coverage Options
UnitedHealthcare Medicare Advantage Plans will likely offer a variety of coverage options, but it’s important to understand the potential limitations that may apply. Coverage options may vary widely by plan and region, meaning that not all benefits may be available to all members. To stay informed, members should regularly review UnitedHealthcare’s Medicare Advantage Medical Policies, which are updated to align with changes from the Centers for Medicare & Medicaid Services (CMS).
Some out-of-network services might incur higher costs. Using network providers could help minimize out-of-pocket expenses and possibly provide better coverage. Always consult your healthcare provider regarding care decisions, as the Medicare Advantage Medical Policies serve only as informational resources.
Prescription Drug Coverage

Some UnitedHealthcare Medicare Advantage Plans may integrate prescription drug coverage, which could potentially reduce prescription drug costs for Medicare beneficiaries. Certain certain medications may have lower copays during specific coverage phases, but this may vary based on the formulary.
Access to Healthcare Services and Providers

Access to healthcare services and providers has been a cornerstone of UnitedHealthcare Medicare Advantage Plans. Members could access a variety of potential healthcare services through a robust network of providers, likely ensuring convenience and quality care. Whether you need to see a specialist, visit a hospital, or receive outpatient care, the network has been designed to meet diverse healthcare needs.
Using network providers could potentially reduce certain out-of-pocket costs and enhance coverage. The network likely includes various specialists, hospitals, and outpatient facilities, making it easier for members to receive the care they need without unnecessary financial burdens.
How to Enroll in UnitedHealthcare Medicare Advantage Plans
Enrolling in UnitedHealthcare Medicare Advantage Plans is a straightforward process, but it’s essential to be aware of the specific enrollment periods. The Annual Enrollment Period runs from October 15 to December 7 each year, during which individuals can sign up for or make changes to their plans. Enrollment requires necessary documentation such as the Medicare number and relevant personal identification information.
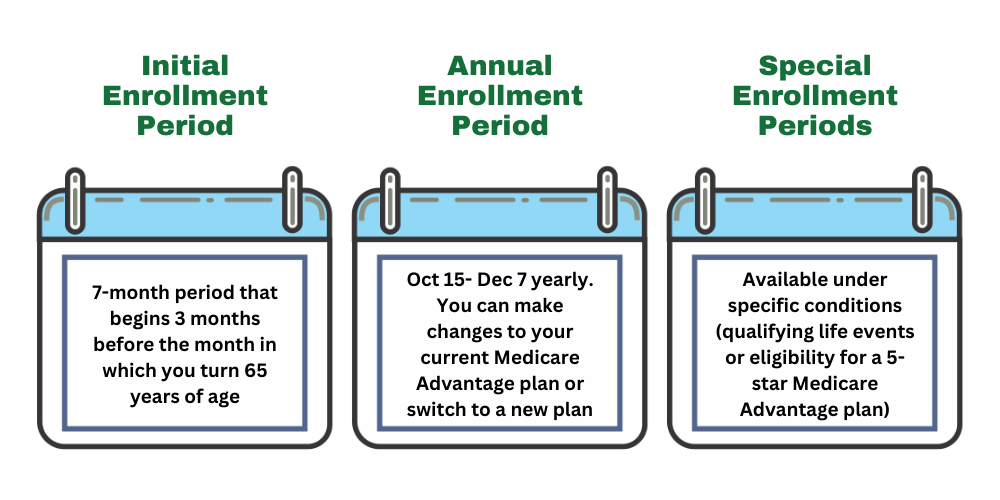
New enrollees may also need to specify their preferred plan option and provide details about their healthcare needs during the application process. Beneficiaries can enroll through this website or by calling one of our licensed agents using the number on this website.
Review the plan’s coverage details and potential benefits to ensure alignment with individual healthcare needs before finalizing enrollment.
Reviewing Your Plan Annually
An annual review of your Medicare plan ensures it continues to meet your healthcare needs. Potential benefits and coverage options might change each year, making it essential to stay informed. Failing to review your plan might lead to financial consequences, with some individuals overspending annually due to inappropriate plan selections.
The Annual Open Enrollment Period, from October 15 to December 7, is the ideal time to review your Medicare plans. A thorough annual review can be completed in about 10 to 15 minutes by asking a few key questions regarding your health needs and provider networks. This ensures that you are making the best decisions for your healthcare.
Summary
The UnitedHealthcare Medicare Advantage Plans in South Dakota for 2026 will likely offer a comprehensive range of potential benefits that could help meet the diverse healthcare needs of enrollees. From essential medical services and occasionally prescription drug coverage to potential health benefits, these plans could provide valuable support for your health journey. Reviewing your plan annually and staying informed about possible changes is crucial to maximizing your potential benefits. Make informed decisions and take control of your healthcare with UnitedHealthcare Medicare Advantage Plans.
Frequently Asked Questions
→ What change may occur regarding the coverage gap phase in 2026?
Unfortunate, the plan details for 2026 have not been released, but make sure to check back in to this article/website for updated information for the 2026 calendar year.
→ What are the enrollment periods for UnitedHealthcare Medicare Advantage Plans?
UnitedHealthcare Medicare Advantage Plans have specific enrollment periods: the Initial Enrollment Period, the Annual Enrollment Period from October 15 to December 7, the Open Enrollment Period from January 1 to March 31, and Special Enrollment Periods for qualifying events. It’s essential to be aware of these dates to ensure proper enrollment.
→ What additional benefits could UnitedHealthcare Medicare Advantage Plans 2026 provide compared to Original Medicare?
Some Untiedhealthcare Medicare Advantage Plans might provide additional benefits such as dental, vision, and hearing care, and sometimes integrate prescription drug coverage, possibly enhancing overall healthcare support compared to Original Medicare.
→ How might out-of-pocket maximums work with UnitedHealthcare Medicare Advantage Plans?
Out-of-pocket maximums could limit the total expenses members pay for covered services within a plan year, possibly ensuring financial protection against high medical costs. This potential feature could provide peace of mind when managing healthcare expenses.

ZRN Health & Financial Services, LLC, a Texas limited liability company



