Humana Medicare Advantage Plans Wisconsin 2026
Looking for detailed insights into the potential Humana Medicare Advantage plans in Wisconsin for 2026? This article covers everything you need to know, from the types of plans available to possible updates and potential benefits. Stay informed and make the best choice for your healthcare needs.
Key Takeaways
- Humana offers a range of Medicare Advantage plans in Wisconsin, including HMO, PPO, and SNP plans, each tailored to different healthcare needs.
- Enrollees could potentially benefit from comprehensive coverage such as dental, vision, and hearing services, and sometimes prescription drug coverage.
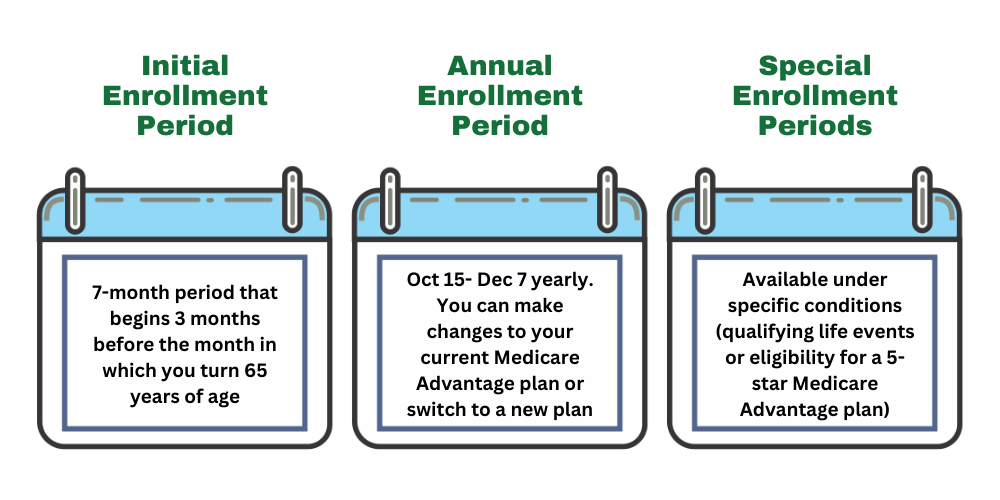
- Enrollment periods, including Initial and Annual Enrollment, are critical for beneficiaries to understand to avoid penalties and ensure coverage continuity.
Compare Plans in One Step!
Enter Zip Code
Humana Medicare Advantage Plans Overview for Wisconsin in 2026
Humana will likely offer a variety of Medicare Advantage plans in Wisconsin, each designed to cater to different healthcare needs. These plans include Health Maintenance Organization (HMO), Preferred Provider Organization (PPO), and Special Needs Plans (SNP), each with its unique features and benefits.
HMO Plans
Humana’s HMO plans are structured to provide comprehensive care while keeping costs manageable. Enrollees are required to select a primary care physician (PCP) who will coordinate all their healthcare needs. This means any specialty care will need a referral from the PCP, likely ensuring that all aspects of care are well-managed and integrated.
The necessity of using a network of approved doctors and hospitals under HMO plans could help control costs and maintain quality. Though the network restriction may seem limiting, it ensures consistent and high-quality care. This coordination could be especially beneficial for managing chronic conditions and preventing potential health issues from escalating.
PPO Plans
Humana’s PPO plans offer more flexibility compared to HMO plans, allowing enrollees to see any healthcare provider, whether in-network or out-of-network, without needing referrals. This flexibility may be particularly beneficial for those who travel frequently or live in areas where access to in-network providers may be limited. Keep in mind that choosing out-of-network providers generally results in higher out-of-pocket costs.
While some PPO plans might come with higher premiums compared to HMO plans, they provide greater freedom in choosing healthcare providers and potentially higher costs for out-of-network services. This trade-off between cost and flexibility likely makes PPO plans an attractive option for those who prioritize choice and convenience in their medical care.
SNP Plans
Special Needs Plans (SNPs) offered by Humana are tailored for individuals with specific chronic conditions, providing customized care and benefits to meet their unique health needs. These plans ensure that beneficiaries receive coordinated and specialized care, which is critical for managing complex health issues effectively.
The focus on tailored benefits and care coordination could make SNPs a robust option for those requiring more personalized health management.
Possible Changes to Humana Medicare Advantage Plans in 2026
Unfortunately, there is currently no information about possible changes or updates for the Humana Medicare Advantage plans for 2026 because the plan details have not been released yet. However, make sure to check back into this article/website for updated information for the 2026 calendar year.
Possible Benefits and Services
Some Humana Medicare Advantage plans may offer enhanced benefits and services designed to promote comprehensive health management. These benefits might include dental, vision, and hearing coverage, underlining Humana’s commitment to preventive care, helping enrollees detect and address health issues early.
Taking advantage of these potential health benefits likely ensures beneficiaries could receive comprehensive care, aligning with their health needs and lifestyle.
Enrollment Process and Deadlines
Enrolling in Humana Medicare Advantage plans in Wisconsin involves specific steps and documentation. Applicants need to provide proof of their Medicare eligibility and residency, which includes various forms of identification and eligibility documentation.
Meeting the required deadlines and understanding the enrollment process ensures coverage without interruptions.
Initial Enrollment Period
The Initial Enrollment Period (IEP) for Medicare beneficiaries is a critical timeframe that lasts seven months. It begins three months before an individual’s 65th birthday, includes the birthday month, and extends three months after. This period is essential for first-time Medicare beneficiaries to enroll in plans without penalties.
Timely enrollment during this period helps avoid gaps in coverage and potential late enrollment penalties.
Annual Enrollment Period
The Annual Enrollment Period (AEP) occurs from October 15 to December 7 each year. This period provides an opportunity for beneficiaries to:
- Review their Medicare plans
- Switch plans
- Adjust coverage
- Return to Original Medicare without facing penalties
This flexibility allows beneficiaries to adapt their coverage to better meet their changing health needs and preferences.
Special Enrollment Periods
Special Enrollment Periods (SEPs) are available for beneficiaries who experience significant life changes, such as relocating or losing other health insurance coverage. These periods allow individuals to enroll in or switch plans outside the standard enrollment periods.
Knowing the conditions that qualify for SEPs offers additional flexibility and ensures continuous coverage during transitional life events.
Comparing Humana Medicare Advantage Plans with Original Medicare

When deciding between Humana Medicare Advantage Plans and Original Medicare, understanding the differences in coverage, costs, and potential benefits is crucial. Some of Humana’s plans may offer more comprehensive coverage and additional services that might not be included in Original Medicare.
The following is a detailed comparison to assist in making an informed decision.
Coverage Differences
One of the potential distinctions between Humana Medicare Advantage plans and Original Medicare will likely be the scope of coverage. Some of the Humana plans may integrate prescription drug coverage, which covers certain medications under Part D.
Moreover, some Humana plans may also cover services like vision, dental, and hearing, which are not included under Original Medicare. These potential benefits likely ensure that beneficiaries could receive comprehensive care that addresses various aspects of their health.
Cost Comparison
The cost structures of some Humana Medicare Advantage plans may differ from Original Medicare. Certain Humana plans might feature out-of-pocket costs that could vary based on the specific plan selected, such as premiums and deductibles. However, choosing in-network providers could potentially lower these out-of-pocket expenses, possibly making healthcare more affordable.
Unlike the standardized cost structure of Original Medicare, some Humana plans may also incorporate cost-sharing mechanisms such as lower copayments for certain services, which could potentially reduce overall healthcare costs for beneficiaries. This flexibility in cost management could be a significant advantage for those looking to balance comprehensive coverage with affordability.
How to Maximize Your Possible Benefits with Humana Medicare Advantage Plans

To get the most out of your Humana Medicare Advantage plan, it’s essential to understand how to utilize the available resources effectively. This will likely include choosing in-network providers and taking advantage of the potential preventive care services.
This approach likely ensures beneficiaries receive comprehensive care while potentially minimizing out-of-pocket costs.
Utilizing Network Providers
Using in-network providers is a critical strategy for maximizing your potential benefits under certain Humana Medicare Advantage plans. In-network providers may result in lower copayments and coinsurance, possibly reducing healthcare expenses compared to using out-of-network providers. This could be particularly beneficial in rural areas where access to healthcare providers may otherwise be limited.
Humana will likely offer HMO plans that require members to use a network of doctors and hospitals, while PPO plans may provide more flexibility, including the option to see out-of-network providers at a higher cost. Understanding these differences could help you choose the plan that best fits your healthcare needs and financial situation.
Customer Support and Resources
Humana provides robust customer support and resources to help beneficiaries navigate their Medicare Advantage plans. Members can reach out to customer service for assistance with plan inquiries and support, ensuring they have the information needed to make the most of their benefits.
Access to these resources is crucial for addressing any questions or concerns that may arise.
Online Tools and Resources
By entering your zip code into the Plan Finder Tool on this website, members can manage their plans effectively. Our Plan Finder Tool allows members to find in-network doctors and healthcare providers, as well as compare costs and coverage options.
This online resource is invaluable for navigating healthcare options and making informed decisions.
Summary
Humana Medicare Advantage plans in Wisconsin for 2026 will likely offer a range of options tailored to meet diverse healthcare needs. The potential benefits might make these plans an attractive choice for many beneficiaries. By understanding the enrollment process, comparing plan options, and utilizing available resources, you can ensure you make the most informed decision for your health and well-being. Stay proactive, engage in preventive care, and take advantage of the comprehensive support Humana provides.
Frequently Asked Questions
→ What types of Humana Medicare Advantage plans are available in Wisconsin?
Humana Medicare Advantage plans available in Wisconsin include HMO, PPO, and SNP options, catering to various healthcare requirements. It’s important to choose the plan that best fits your specific needs.
→ What are the possible changes for Humana Medicare Advantage plans in 2026?
Unfortuantly, the plan details for 2026 have not been released, but make sure to check back in to this article/website for updated information for the 2026 calendar year.
→ What is the Initial Enrollment Period for Medicare beneficiaries?
The Initial Enrollment Period for Medicare beneficiaries spans seven months, beginning three months before and ending three months after an individual’s 65th birthday. It’s crucial to note these dates to ensure you receive your Medicare coverage on time.
→ What additional benefits could Humana Medicare Advantage plans offer over Original Medicare?
Some Humana Medicare Advantage plans might provide additional benefits like dental, vision, and hearing coverage, possibly enhancing coverage beyond what Original Medicare offers.

ZRN Health & Financial Services, LLC, a Texas limited liability company