Humana Medicare Advantage Plans Illinois 2026
Wondering about the potential Humana Medicare Advantage plans in Illinois for 2026? This article covers the HMO, PPO, and SNP options, along with potential plan benefits. Understand how these plans could fit your healthcare needs.
Key Takeaways
- Humana will likely offer a variety of Medicare Advantage plans in Illinois for 2026, including HMO, PPO, and Special Needs Plans, catering to diverse healthcare needs.
- Star ratings could significantly impact plan quality assessments, with Humana facing an increase in ratings, indicating excellent member satisfaction and financial stability.
- Some Humana plans might offer additional benefits such as dental, vision, and hearing coverage, and sometimes prescription drug coverage.
Compare Plans in One Step!
Enter Zip Code
Overview of Humana Medicare Advantage Plans in Illinois for 2026

Humana offers a diverse range of Medicare Advantage plans in Illinois for 2026, catering to the varied healthcare needs of Medicare beneficiaries. These plans include Health Maintenance Organization (HMO) plans, Preferred Provider Organization (PPO) plans, and Special Needs Plans (SNP).
Whether you prefer the coordinated care of an HMO, the flexibility of a PPO, or the specialized services of an SNP, Humana has a plan to meet your healthcare requirements.
HMO Plans
Humana’s HMO plans are designed to promote coordinated care by requiring members to select a primary care physician who manages their overall healthcare. This arrangement could ensure members receive necessary referrals for specialist care, effectively managing their healthcare needs.
HMO plans generally offer lower costs compared to other plan types, possibly making them attractive to many. However, members must stay within the plan’s network of doctors and hospitals, except in emergencies.
PPO Plans
Humana’s PPO plans provide greater flexibility, enabling members to visit any healthcare provider without referrals, albeit with higher premiums. Members may also access a broader range of providers, including out-of-network services, at a higher cost.
This flexibility could be valuable for those who prefer not to be limited by a referral system, making PPO plans a suitable choice for those willing to pay higher premiums for extended access.
SNP Plans
Humana’s Special Needs Plans (SNPs) are tailored for individuals with specific chronic conditions or those eligible for both Medicare and Medicaid. These plans offer specialized care and services to meet the unique healthcare needs of these populations, ensuring they receive the necessary attention and management for their conditions.
Potential Changes to Medicare Advantage Plans in 2026
There is currently no information about the potential plan changes for 2026 because the plan details have not been released. However, make sure to check back into this website for updated information for the 2026 calendar year.
CMS Regulations
The Centers for Medicare & Medicaid Services (CMS) regulations will likely ensure that Medicare Advantage plans cover all necessary Medicare Part A and B benefits. These regulations may limit cost-sharing for certain services to levels comparable to Traditional Medicare.
These regulations may also provide enhanced accessibility of provider directory information via the Plan Finder tool on this website.
Star Ratings and Their Importance

Star ratings could help Medicare beneficiaries choose high-quality Medicare Advantage plans. These ratings, determined by various performance metrics, reflect the quality of care provided by the plans. Higher star ratings can indicate better plan offerings and member satisfaction, guiding potential enrollees.
CMS regulations aim to improve the quality of Medicare Advantage plans, likely influencing these performance metrics.
Understanding Star Ratings
The star rating system evaluates Medicare Advantage plans using a scale from one to five stars to indicate their quality. CMS evaluates these plans based on up to 40 quality and performance metrics, including various factors like member satisfaction, chronic condition management, and preventive services.
These star ratings are updated yearly in September, aligning with the Medicare open enrollment period.
Humana’s Performance
Based on data from recent years, it is estimated that approximately 94% of Humana’s members were enrolled in plans rated four stars or higher. These star ratings could improve Humana’s financial stability, potentially increasing member benefits.
Humana will likely implement performance improvements that could enhance future star ratings.
Potential Benefits and Coverage Options

Some of Humana’s Medicare Advantage plans may offer a variety of benefits tailored for Illinois residents. Certain plans may include comprehensive health services supported by a coordinated network of hospitals, doctors, and pharmacies.
These potential benefits will likely provide robust coverage and improve healthcare outcomes for beneficiaries.
Additional Benefits
Some of Humana’s Medicare Advantage plans may offer additional health benefits, including dental, vision, and hearing coverage designed to improve overall health. These potential benefits will likely support various aspects of health management, possibly ensuring beneficiaries receive necessary care.
Enrollment Process and Deadlines
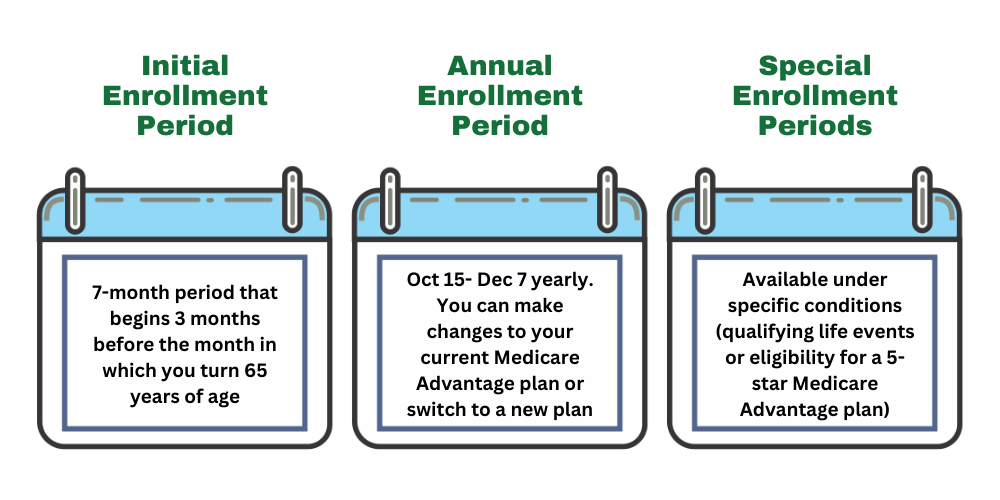
Understanding the enrollment process and deadlines is crucial for maximizing Humana Medicare Advantage plans. Multiple enrollment periods exist, including the Initial Enrollment Period, the Annual Election Period, and Special Enrollment Periods. Each period offers different opportunities to join or switch plans to meet healthcare needs.
Initial Enrollment Period
The Initial Enrollment Period is a seven-month window starting three months before an individual turns 65 and ending three months after their birthday. This period is essential for first-time enrollees to apply for Humana Medicare Advantage plans, ensuring coverage as soon as they are eligible.
Annual Election Period
The Annual Election Period occurs each year from October 15 to December 7. During this period, beneficiaries can switch plans, enroll in a new plan, or drop existing coverage.
Medicare recipients should review their coverage annually to ensure it continues to meet their healthcare needs, especially as plan benefits and costs might change.
Special Enrollment Periods
Special Enrollment Periods allow beneficiaries to enroll in Medicare Advantage plans outside standard enrollment periods due to qualifying life events. Such events include moving to a new address or losing other health coverage.
These periods ensure beneficiaries can maintain healthcare coverage despite changes in circumstances.
Comparing Potential Costs and Premiums
When choosing a Humana Medicare Advantage plan, comparing the possible costs and premiums may be essential. Some plans may include premiums, deductibles, and out-of-pocket maximums, which could significantly affect overall healthcare expenses.
Understanding these costs could help beneficiaries make informed healthcare decisions.
Premium Breakdown
Monthly premiums for certain Humana Medicare Advantage plans may vary depending on the selected plan type. Some plans may offer low premiums, possibly providing cost-effective options.
Evaluating and understanding these potential premium costs could help make an informed choice about Medicare Advantage plans.
Deductibles and Out-of-Pocket Costs
Certain Humana Medicare Advantage plans may feature specific deductibles that beneficiaries must meet before coverage starts, along with potential annual out-of-pocket maximums that could limit total spending. These potential out-of-pocket maximums could protect beneficiaries from excessive healthcare costs by capping total spending for covered services.
Network and Provider Access
Humana will likely offer a comprehensive network of hospitals, doctors, and pharmacies accessible to Medicare Advantage members. This network might include various providers, possibly allowing members to receive treatment from local hospitals, primary care physicians, and a wide range of pharmacies.
Members will likely be able to access specialists through referrals from primary care doctors within the network, likely ensuring streamlined care coordination.
Plan’s Network
Humana offers HMO and PPO plans as part of its Medicare Advantage offerings in Illinois, each with distinctive network structures. HMO plans require members to choose a primary care physician and obtain referrals to see specialists within the network, limiting out-of-network care options. Conversely, PPO plans provide greater flexibility, allowing members to see any doctor or specialist, though at a higher cost for out-of-network services.
Both plan types may have limitations on out-of-network service coverage, affecting the total healthcare options available.
Access to Specialists
Some Humana Medicare Advantage plans may offer beneficiaries access to a wide range of specialists. However, access to specialists may be limited by the plan’s network, particularly in HMO plans requiring referrals to see certain specialists.
Beneficiaries may encounter service gaps when trying to access specialists outside their plan’s network, potentially leading to higher costs or denied services.
Navigating Plan Changes
To effectively adjust to potential changes in benefits, members should regularly review communication from their plan, particularly during the Annual Notice of Change.
Additionally, some Humana plans might appeal certain star rating results, which could improve member plan options and mitigate negative changes, particularly in light of higher industry cut points.
Addressing Service Gaps
Strategies such as appealing coverage denials and seeking alternative providers may also help members manage gaps in medical service access. Accessing necessary medical services may require members to actively seek alternative providers if their current coverage limits their options.
Addressing service gaps may also be crucial for members to receive the healthcare services they need.
Summary
The Humana Medicare Advantage plans in Illinois for 2026 will likely be shaped by a variety of factors, including star ratings and an array of potential benefits. Understanding these elements will likely be essential for making informed decisions about your healthcare. From HMO and PPO plans to SNPs, Humana offers a range of options designed to meet diverse healthcare needs.
Staying informed about potential changes is crucial. By understanding the enrollment process, comparing possible costs, and navigating challenges, beneficiaries could maximize their healthcare benefits. As you consider your options, keep in mind the importance of star ratings and the comprehensive benefits that Humana’s plans provide.
Frequently Asked Questions
→ What types of Medicare Advantage plans does Humana offer in Illinois?
Humana offers Health Maintenance Organization (HMO), Preferred Provider Organization (PPO), and Special Needs Plans (SNP) in Illinois, providing a range of options to meet various healthcare needs.
→ What are the key enrollment periods for Medicare Advantage plans?
The key enrollment periods for Medicare Advantage plans are the Initial Enrollment Period, the Annual Election Period, and Special Enrollment Periods, providing essential opportunities to enroll or change plans. Make sure to mark these dates to secure your coverage effectively.
→ What is the significance of star ratings in choosing Medicare Advantage plans?
Star ratings could be crucial in choosing Medicare Advantage plans as they reflect the quality and performance of the plans, helping beneficiaries make informed decisions for better health outcomes. Prioritizing plans with higher ratings could lead to access to superior care and services.
→ What strategies could help address service gaps in Humana Medicare Advantage plans?
To effectively address service gaps in certain Humana Medicare Advantage plans, members should appeal coverage denials, explore alternative providers, and ensure clear communication about any plan changes. Taking these steps could help you navigate and improve your overall healthcare experience.

ZRN Health & Financial Services, LLC, a Texas limited liability company




