Healthcare Medicare Advantage Plans 2026
Major changes will likely be coming to Healthcare Medicare Advantage plans
Key Takeaways
- Significant regulatory changes
in 2026 could enhance protections for Medicare Advantage Plans and possibly improve coordination with Medicaid, particularly through new regulations on agent compensation and streamlined appeals processes.
- The Medicare Advantage market is highly concentrated, with UnitedHealthcare, Humana, and CVS Health dominating enrollment; their influence will likely continue shaping offerings and accessibility for beneficiaries.
- Potential changes
in 2026 may include a cap on out-of-pocket drug costs, possible expansions in dental and behavioral health services, and improved drug coverage, all will likely be aimed at enhancing affordability and comprehensive care for beneficiaries.
Compare Plans in One Step!
Enter Zip Code
Possible Changes to Medicare Advantage Plans in 2026

The year
Another update may be the requirement for Fully Integrated Dual Eligible Special Needs Plans (FIDE SNPs) to have exclusively aligned enrollment starting in 2025. This change will likely be designed to improve coordination between Medicare and Medicaid, ultimately benefiting the beneficiaries.
These regulatory changes will likely highlight a commitment to enhancing the Medicare program and ensuring better, more integrated care from Medicare Advantage Plans.
Dominant Providers in the Medicare Advantage Market
The Medicare Advantage market has been dominated by a few providers in recent years. UnitedHealthcare and Humana together accounted for about 47% of all Medicare Advantage enrollment across the United States in 2023. This concentration likely highlights the significant influence these companies could have in shaping the market and determining the offerings available to beneficiaries. Notably, UnitedHealthcare’s enrollment share increased from 20% in 2010 to 29% in 2024, demonstrating substantial growth over the years.
CVS Health, following its acquisition of Aetna, has also had a remarkable rise in its market share, doubling from 6% in 2010 to 12% in 2022. The combined market presence of UnitedHealthcare, Humana, and CVS Health likely underscores the competitive nature of Medicare Advantage Plans and the importance of these providers in delivering comprehensive care to older adults.
Looking ahead, these providers will likely continue shaping the future of Medicare Advantage.
Impact of the Inflation Reduction Act on Medicare Advantage
The Inflation Reduction Act will likely have a profound impact on Medicare Advantage Plans, particularly in terms of drug coverage. Starting
Moreover, the Centers for Medicare & Medicaid Services (CMS) may also publicly disclose the negotiated prices by March 2025, which could promote transparency and allow beneficiaries to make more informed decisions about their drug plans.
The Act may also mandate that pharmaceutical companies reimburse Medicare if their drug prices rise faster than inflation, possibly ensuring cost control and preventing unjustified price hikes. These measures will likely collectively aim to reduce premium increases and enhance the overall affordability of healthcare for Medicare beneficiaries.
Enhanced Behavioral Health Services
Enhancements in behavioral health services might be a significant focus for certain Medicare Advantage Plans
Evaluating the addition of behavioral health providers could help Medicare Advantage Plans meet specific service delivery criteria and maintain high-quality care. These updates may also reflect a broader commitment to enhancing behavioral health services and supporting the mental well-being of beneficiaries.
Prescription Drug Coverage Changes

Prescription drug coverage under Medicare Advantage Plans may also see significant changes
Furthermore, the various costs that count towards the catastrophic coverage threshold may include out-of-pocket expenses during the deductible and initial coverage phases, along with partial costs during the coverage gap. This adjustment could potentially ensure that beneficiaries reach the catastrophic phase more predictably.
These potential changes reflect a commitment to improving drug coverage and reducing out-of-pocket expenses for Medicare beneficiaries.
Comprehensive Dental Coverage Additions
Some Medicare Advantage Plans
New policies may also facilitate coverage for additional services such as dentures and oral surgery, further broadening the scope of dental care available under Medicare Advantage Plans. Improved coordination between dental and overall health services may also promote holistic care and enhance beneficiary well-being.
Comprehensive dental coverage could reflect a commitment to offering more inclusive and supportive healthcare options.
New Out-of-Pocket Cost Caps
Another potential change in Medicare Advantage Plans
The new out-of-pocket cost caps reflect a broader effort to reduce financial barriers and enhance the affordability of healthcare.
How to Compare Medicare Advantage Plans
Comparing Medicare Advantage Plans is crucial for finding the most suitable option for individual healthcare needs. When evaluating plans, it’s important to consider both potential costs and benefits to ensure they meet your specific healthcare requirements. Understanding the possible out-of-pocket costs, such as deductibles and copayments, is vital for making informed comparisons between plans.

Utilizing tools like this website can help beneficiaries evaluate and compare the quality of different Medicare Advantage Plans based on their Star Ratings. Additionally, reviewing performance measures and feedback from current enrollees could also provide insights into the quality of care and service offered by different plans.
By carefully comparing plans, beneficiaries can make informed decisions and select the best plan for their healthcare needs.
The Role of Medicaid Services in Medicare Advantage
Medicaid services play a crucial role in Medicare Advantage Plans, particularly for dual-eligible individuals. Starting
In 2021, a significant portion of dual-eligible individuals received Medicaid and Medicare benefits through separate systems, highlighting the complexity of their coverage landscape. By increasing enrollment in affiliated managed care plans, the new rule will likely aim to streamline services and improve care coordination for dually eligible individuals.
These potential updates reflect a commitment to enhancing the possible integration of Medicaid services within Medicare Advantage Plans and supporting the unique needs of dual-eligible beneficiaries.
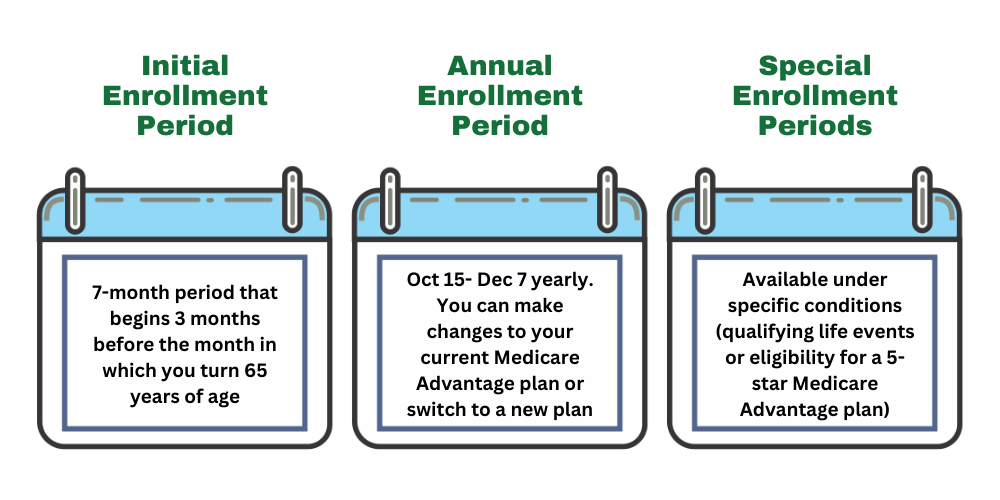
Preparing for the Annual Enrollment Period
The Annual Enrollment Period for Medicare is a critical time for beneficiaries to review and modify their health plans.
By entering your zip code into this website, members can compare monthly expenses across different plans. Additionally, personalized guidance is available through in-person counseling from local State Health Insurance Assistance Programs (SHIP), providing valuable support during the enrollment period.
Preparing for the Annual Enrollment Period ensures that beneficiaries can select the best plan for their healthcare needs.
Understanding the Initial Coverage Phase and Catastrophic Phase
Understanding the phases of Medicare Part D coverage is essential for managing prescription drug costs. In the initial coverage period, after meeting the deductible, the Medicare Part D plan may share the costs of prescription drugs with the beneficiary until their total drug costs reach a specified limit. This phase could help beneficiaries manage their expenses and provide predictable coverage for prescription medications.
Knowing these phases could aid beneficiaries in planning their healthcare expenses and maximizing their prescription drug coverage.
Other Medicare Changes for 2026
The year
Additionally, starting in 2025, individuals with Medicare Part D may also benefit from a yearly limit on out-of-pocket costs for prescription drugs, possibly further enhancing affordability and access to necessary medications. These changes likely highlight the ongoing efforts to improve the Medicare program and could provide better support for Medicare beneficiaries.
Summary
The potential changes coming to Medicare Advantage Plans
As we look ahead, it’s essential for beneficiaries to stay informed and take advantage of the tools and resources available to make the best healthcare decisions. By understanding the possible changes and preparing for the Annual Enrollment Period, beneficiaries can ensure they select the most suitable plan for their needs. These efforts collectively aim to create a more supportive and effective healthcare system for all Medicare beneficiaries.
Frequently Asked Questions
→ What is the new out-of-pocket cost cap for Medicare Part D in 2026 ?
The plan benefits have not been released, but make sure to check back in to this article/website for updated information for the
→ How will the Inflation Reduction Act impact Medicare Advantage Plans?
The plan benefits have not been released, but make sure to check back in to this article/website for updated information for the
→ What are the new enhancements in behavioral health services for Medicare Advantage Plans?
The new enhancements in behavioral health services for Medicare Advantage Plans might feature updated network adequacy standards that may incorporate more mental health providers. These potential changes likely aim to improve access to necessary care for beneficiaries.
→ How can beneficiaries compare different Medicare Advantage Plans?
Beneficiaries can effectively compare different Medicare Advantage Plans by using this website, which allows them to evaluate costs, possible benefits, and quality through Star Ratings. This provides a clear overview to make informed decisions about their healthcare options.
→ What are the potential changes in prescription drug coverage for 2026 ?
Some of the potential changes to prescription drug coverage

ZRN Health & Financial Services, LLC, a Texas limited liability company



