Health Net Medicare Advantage Plans 2026
What potential changes could you expect from Health Net Medicare Advantage Plans
Key Takeaways
- Health Net will likely expand its Medicare Advantage plans
for 2026 , possibly introducing new options and improved pricing for medications to enhance coverage for beneficiaries.
- The plans will likely offer a variety of types, including HMOs, PPOs, and SNPs, which may provide supplemental benefits such as dental, vision, and hearing coverage.
- Enrollment for the new plans will be available during the Annual Enrollment Period from October 15 to December 7, with crucial steps to ensure beneficiaries choose the most suitable options.
Compare Plans in One Step!
Enter Zip Code
Overview of Health Net Medicare Advantage Plans 2026
Health Net will likely expand its Medicare Advantage offerings
One possible change in the
Incorporating beneficiary feedback, Health Net will likely aim to enhance the member experience and ensure robust healthcare coverage.
Plan Options
Health Net’s Medicare Advantage plans will likely be designed to cater to a wide range of healthcare needs, possibly ensuring that there’s something for everyone. These plans include Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), and Special Needs Plans (SNPs). Each type of plan offers unique benefits and coverage options, allowing beneficiaries to choose the one that best matches their healthcare preferences and requirements.
The variety in plan types might not only increase transparency but could also provide flexibility for enrollees. Whether you prefer a more structured network with an HMO, the flexibility of a PPO, or the specialized care of an SNP, Health Net aims to meet your needs.
Each plan type is intended to cover various services, and costs may vary accordingly. It’s crucial to determine which health plan best fits your medical needs and financial situation for the upcoming plan year.
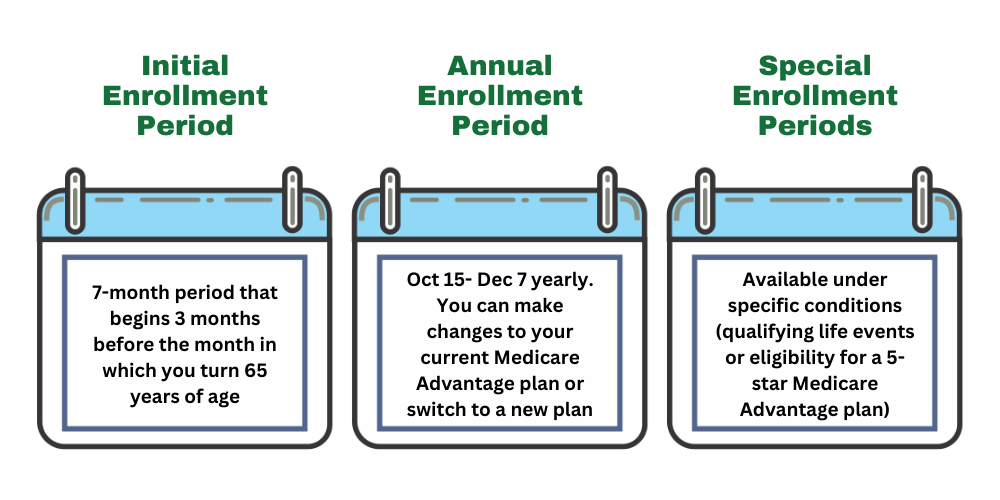
Enrollment Process
Awareness of specific enrollment periods is crucial for enrolling in Health Net Medicare Advantage plans. The Annual Enrollment Period (AEP) runs from October 15 to December 7 each year, during which time you can enroll in or switch Medicare Advantage plans. If you miss the AEP, you may have to wait until the next enrollment period or qualify for a Special Enrollment Period (SEP) due to certain circumstances.
The enrollment process involves several steps, including reviewing your current Medicare plan, exploring other options, and completing an application for the new plan. Adhering to these timelines and deadlines could help avoid potential late enrollment penalties or delays in coverage.
Current enrollees should assess their healthcare needs and the possible benefits provided by different plans before making a decision.
Eligibility Criteria
Eligibility for Health Net Medicare Advantage plans generally requires individuals to be aged 65 or older. However, those under 65 who receive Social Security Disability Benefits are also eligible. Additionally, beneficiaries must be enrolled in both Medicare Part A and Part B to qualify for these plans.
Certain categories of individuals, such as those with specific disabilities or those who qualify for dual eligible special needs plans, may also be eligible. Older adults and others looking to benefit from comprehensive coverage and services should understand these criteria.
Meeting these eligibility requirements facilitates a smooth enrollment process and access to necessary benefits.
Possible Benefits in Health Net Medicare Advantage Plans

Some of Health Net’s Medicare Advantage plans
Dental Coverage
Dental coverage under certain Health Net’s Medicare Advantage plans may include a range of preventive and comprehensive services. These services will likely cover routine check-ups, cleanings, and certain surgical procedures, possibly ensuring that members can maintain good oral health.
In addition to preventive services, Health Net’s dental coverage may also include restorative procedures and oral surgeries that are deemed medically necessary. This comprehensive approach to dental care could help address health disparities and could potentially ensure that all Medicare Advantage enrollees receive the dental care they need.
Vision and Hearing Benefits
Some of Health Net’s Medicare Advantage plans may also include robust vision and hearing benefits that cater to the needs of Medicare beneficiaries. Vision benefits might cover routine eye exams, glasses, and contact lenses, possibly ensuring that members could have access to necessary eye care services. These benefits are designed to help detect and treat vision problems early, contributing to better overall health outcomes.
Hearing benefits might include coverage for hearing aids and related services, addressing the hearing needs of enrollees. By potentially including these supplemental benefits, Health Net likely aims to provide comprehensive healthcare that addresses all aspects of members’ well-being.
These potential benefits could also enhance standard Medicare coverage and possibly ensure enrollees have better access to essential health services, leading to improved health outcomes.
Drug Coverage Under Health Net Medicare Advantage Plans

Some Health Net’s Medicare Advantage plans may offer comprehensive prescription drug coverage. By potentially integrating this coverage with Medicare benefits, this drug coverage could potentially ensure that beneficiaries have access to a wide variety of necessary medications. These plans will likely be designed to simplify the process of obtaining prescription drugs, potentially making it convenient for members to manage their health conditions effectively.
The potential inclusion of specific drugs negotiated for pricing under Medicare could significantly impact the formulary of covered drugs, which may ensure that members could receive cost-effective medication options. This possible integration of comprehensive drug coverage within a Medicare Advantage plan could also simplify the overall healthcare experience for enrollees, possibly providing them with seamless access to their prescription benefits.
Part D Coverage
Medicare Part D could be an integral component of Health Net’s Medicare Advantage plans, potentially providing beneficiaries with structured and subsidized access to prescription drugs. This potential integration could simplify coverage, allowing members to access their prescription benefits seamlessly.
Managing Prescription Costs
Managing prescription costs is a critical concern for many Medicare Advantage enrollees. Health Net could offer several strategies that might help beneficiaries lower their out-of-pocket expenses for medications. These strategies may include using generic alternatives, participating in drug discount programs, and utilizing mail-order services for long-term medications. Opting for generic medications and reviewing plan options could also significantly reduce prescription expenses for members.
Additionally, optional payment plans might allow beneficiaries to distribute their medication costs over several months, possibly easing the financial burden of expensive prescriptions. These strategies are designed to help Medicare Advantage enrollees manage their healthcare costs more effectively, ensuring that they can afford the medications they need to maintain their health.
Comparing Premium Costs
Premium costs for Health Net Medicare Advantage plans
The average monthly premium
Out-of-Pocket Spending Limits

Out-of-pocket spending limits are a crucial feature designed to protect Medicare Advantage enrollees from high medical costs. These limits could potentially ensure that once beneficiaries reach a certain threshold, they do not have to pay additional out-of-pocket expenses for covered services.
Financial assistance programs may also help enrollees with premium costs, possibly ensuring those with lower incomes could access necessary healthcare services.
Financial Assistance Options
Some of Health Net’s Medicare Advantage plans may include annual out-of-pocket spending caps that could potentially safeguard members from excessive medical expenses. These limits will likely be designed to prevent exorbitant costs and provide a financial safety net for enrollees.
Additionally, financial assistance programs will be available to help enrollees manage premium costs and out-of-pocket expenses, possibly ensuring better access to necessary healthcare services.
How to Switch Medicare Advantage Plans
Switching Medicare Advantage plans could be a strategic move for beneficiaries looking to optimize their healthcare coverage. The Medicare Open Enrollment Period, which occurs annually from October 15 to December 7, provides an opportunity for beneficiaries to switch plans or enroll in a new one. Additionally, the Medicare Advantage Open Enrollment Period, from January 1 to March 31, allows changes to coverage for those already enrolled in Medicare Advantage plans.
To switch plans, gather necessary personal information and current plan details, then complete your application for the new plan either through the comparemedicareadvantageplans.org website or by calling us at 1-833-641-4938 (TTY 711), Mon-Fri 8 am-9 pm EST. Understanding the potential penalties and coverage implications is critical before making a decision.
Consider evaluating your current plan’s performance, researching new options, and ensuring that you meet the deadlines to avoid any penalties.
Timing and Deadlines
The Medicare Advantage Open Enrollment Period runs from January 1 to March 31, allowing beneficiaries to make changes to their coverage. During this period, you can switch plans, drop your Medicare Advantage plan, or return to Original Medicare.
Special Enrollment Periods (SEPs) also allow for changes outside the regular enrollment times under specific circumstances, such as moving to a new location or losing other health coverage. It is crucial to adhere to these timing and deadlines to avoid any gaps in coverage or penalties.
If you enroll during the Open Enrollment Period, your coverage will start on January 1, provided your request is received by December 7. For SEPs, beneficiaries typically have two months to make changes after the qualifying event occurs.
Steps to Switch Plans
Switching Medicare Advantage plans involves several steps. First, evaluate your current plan’s performance and determine your healthcare needs. Next, research the available options in your area, considering the health plan and potential drug plan benefits. Once you have selected a new plan, submit your enrollment request to the new Medicare Advantage plan. The new coverage will generally take effect on the first day of the month following the receipt of your request.
After applying for a new plan, your current coverage will end when the new plan begins. Ensure that your new plan meets your healthcare needs and financial situation before switching. Following these steps allows for a seamless transition to a new Medicare Advantage plan that better suits your requirements.
Potential Penalties and Considerations
Switching Medicare Advantage plans could have significant implications for your coverage and out-of-pocket costs. It is essential to understand the potential penalties and other changes that might occur as a result of switching plans. For instance, if you switch outside the designated enrollment periods without a qualifying event, you may face coverage gaps or late enrollment penalties. Therefore, it is crucial to be fully aware of the deadlines and ensure that you submit your enrollment forms on time.
Moreover, when considering switching plans, evaluate the costs and benefits of your current plan versus the new plan. This may include examining premium costs, out-of-pocket expenses, and the range of covered services. By carefully considering these factors, you can make an informed decision that ensures continuous and comprehensive healthcare coverage without incurring unnecessary costs.
Summary
As we look forward to
For those considering switching Medicare Advantage plans, understanding the enrollment process, eligibility criteria, and potential penalties is crucial. By staying informed and adhering to important deadlines, beneficiaries can optimize their healthcare coverage and manage costs effectively. Ultimately, Health Net’s Medicare Advantage plans
Frequently Asked Questions
→ When is the Annual Enrollment Period for Health Net Medicare Advantage plans?
The Annual Enrollment Period for Health Net Medicare Advantage plans is from October 15 to December 7 each year. It’s important to mark these dates to ensure you have the coverage you need.
→ What types of Medicare Advantage plans does Health Net offer?
Health Net offers a variety of Medicare Advantage plans, including Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), and Special Needs Plans (SNPs). This range ensures that you can choose a plan that best fits your healthcare needs.
→ What supplemental benefits may be included in Health Net’s Medicare Advantage plans for 2026 ?
Some Health Net’s Medicare Advantage plans
→ How can I manage my prescription drug costs under Health Net Medicare Advantage plans?
To effectively manage your prescription drug costs under Health Net Medicare Advantage plans, consider opting for generic medications, participating in drug discount programs, and utilizing mail-order services. These strategies could potentially reduce your out-of-pocket expenses.
→ What are the out-of-pocket spending limits for Health Net Medicare Advantage plans?
Some Health Net Medicare Advantage plans may feature annual out-of-pocket spending caps, possibly providing financial protection against high medical costs. This could potentially ensure that members are safeguarded from excessive expenses throughout the year.

ZRN Health & Financial Services, LLC, a Texas limited liability company



