Is WellCare Medicaid or Medicare?
If you’re wondering if WellCare is Medicaid or Medicare, WellCare will likely provide both Medicaid services and Medicare plans.
WellCare could offer a range of healthcare plans under the Medicare Advantage program (also known as Part C) and may even coordinate with Medicaid through Dual Special Needs Plans (D-SNPs) for those eligible for both Medicare and Medicaid. This article will explore how WellCare may operate within these programs, what could make its plans distinctive, and how you could determine the right WellCare plan for your needs.
Key Takeaways
- WellCare will likely offer Medicare Advantage plans that may come with additional benefits like drug, vision, hearing, and dental services, different from the Original Medicare, and cater to individuals over 65 or with specific disabilities.
- Medicaid’s role through WellCare may include providing Dual Special Needs Plans (D-SNPs) for individuals who qualify for both Medicare and Medicaid, potentially offering comprehensive coverage including prescription drugs, dental, vision, and hearing benefits.
- Some of WellCare’s Medicare Advantage plans may be more cost-effective with low monthly premiums, minimal copays, and limited annual out-of-pocket expenses as compared to Original Medicare’s structure.
Compare Plans in One Step!
Enter Zip Code
Deciphering WellCare: Medicare Advantage or Medicaid?
WellCare has established a unique position in the healthcare sector with its diverse Medicare Advantage and Medicaid plans. To gain a better understanding of these potential offerings, this article will break them down. WellCare might partner with Medicare to potentially provide customers with Medicare Part A and Part B benefits through its Medicare Advantage plans.
Some of these plans may be more than just a reiteration of Original Medicare; they could bring valuable additional benefits.
However, WellCare’s involvement with Medicaid might present a different dynamic. Medicaid, a joint federal and state initiative, could aim to assist individuals with limited income and resources in accessing healthcare services that might not be covered by Medicare. WellCare could potentially integrate these Medicaid services into its offerings by providing Dual Special Needs Plans (D-SNPs) for individuals who qualify for both Medicare and Medicaid.
Some of these plans may offer a blend of benefits from both programs and could provide additional Medicare coverage, which may include more services and potentially reduced out-of-pocket costs compared to Original Medicare.
What is Medicare Advantage?
Medicare Advantage, also known as ‘Part C’ or an ‘MA Plan’, could serve as an alternative to Original Medicare. It is a health plan provided by private companies such as WellCare under a contract with Medicare. It encompasses all Original Medicare services and may sometimes include additional coverage such as:
- vision services
- hearing services
- dental services
 Medicare Advantage could potentially offer extensive coverage than Original Medicare. While Original Medicare offers Part A (Hospital Insurance) and Part B (Medical Insurance), some Medicare Advantage plans may go the extra mile to potentially offer additional Medicare Advantage plan benefits, like prescription drug coverage and regular care for dental, vision, and hearing, which may not be provided by Original Medicare.
Medicare Advantage could potentially offer extensive coverage than Original Medicare. While Original Medicare offers Part A (Hospital Insurance) and Part B (Medical Insurance), some Medicare Advantage plans may go the extra mile to potentially offer additional Medicare Advantage plan benefits, like prescription drug coverage and regular care for dental, vision, and hearing, which may not be provided by Original Medicare.
These plans may be available to those who are 65 years of age or older and are U.S. citizens or legal permanent residents for at least five consecutive years.
Understanding Medicaid’s Role with WellCare
Whereas Medicare Advantage plans will likely be designed for individuals above 65 or those with certain disabilities, Medicaid may also extend support to those with limited income and resources. WellCare, as the Medicare brand for Centene Corporation, might provide Dual Special Needs Plans (D-SNPs) that could coordinate with Medicaid coverage.
The management of these plans will likely be carried out through the D-SNP, which may offer plan types such as HMO and PPO that could cater to individual requirements and may even help manage the cost of healthcare.
These Medicaid managed care plans that could be offered by WellCare may be accessible to individuals who meet the eligibility requirements for Medicaid and those who qualify for both Medicare and Medicaid. What might set WellCare’s Medicaid program apart from traditional Medicaid could be that it might provide additional benefits, including:
- Prescription drug coverage
- Dental benefits
- Vision benefits
- Hearing benefits
Dual Eligible Special Needs Plans (D-SNPs)
 One of the potential offerings within WellCare’s portfolio may be the Dual Eligible Special Needs Plans (D-SNPs). These will likely be a specialized category of Medicare Advantage plans intended for individuals who qualify for both Medicare and Medicaid assistance.
One of the potential offerings within WellCare’s portfolio may be the Dual Eligible Special Needs Plans (D-SNPs). These will likely be a specialized category of Medicare Advantage plans intended for individuals who qualify for both Medicare and Medicaid assistance.
These plans have been carefully crafted to address the unique requirements of dual-eligible beneficiaries, possibly providing them with comprehensive coverage akin to Original Medicare along with customized benefits.
One of the potential advantages of D-SNPs provided by WellCare could be that some plans may deliver supplementary support and advantages.
This could significantly aid in the potential reduction of out-of-pocket expenses for beneficiaries. To be eligible for a D-SNP under WellCare, individuals must meet the qualifications for both Medicare and Medicaid.
The Structure of WellCare Medicare Advantage Plans
WellCare will likely provide a variety of Medicare Advantage plans, such as HMO (Health Maintenance Organization) plans, PPO (Preferred Provider Organization) plans, and D-SNPs (Dual Eligible Special Needs Plans). Each plan type offers a unique blend of benefits, catering to different healthcare requirements.
WellCare may also include prescription drug coverage in some of its Medicare Advantage plans, possibly providing members with comprehensive healthcare benefits. This additional coverage could help members save on medication costs and potentially ensure they could have access to the medications they need.
Furthermore, WellCare may also provide a distinct Medicare Part D prescription drug plan for individuals who may require extensive prescription drug coverage.
Some of WellCare’s plans may also offer supplementary benefits, such as:
- Vision
- Dental
- Hearing coverage
These potential benefits could make WellCare’s plans a comprehensive choice for healthcare coverage.
Possible Plan Types and Benefits
Within WellCare’s array of Medicare Advantage plans, you’ll find three main types: HMO, PPO, and Special Needs Plans. Each of these plan types caters to different healthcare needs and preferences.
WellCare’s Advantage HMO plans emphasize accessibility and affordability of care through an extensive network. On the other hand, PPO plans offer a wider coverage range compared to Original Medicare, making them a suitable choice for individuals who often need care outside of their local area. When comparing Medicare Advantage plans, it’s essential to consider these differences to make the best choice for your healthcare needs.
For individuals who qualify for both Medicare and Medicaid, WellCare may offer D-SNPs, which could offer targeted support and additional benefits. It’s worth noting that some of the copays and deductibles may be subject to variation based on the selected WellCare plan type, possibly impacting the overall expenses linked with each plan.
Prescription Drug Coverage in WellCare Plans
Some of WellCare’s Medicare Advantage plans may include some of the following features:
- Prescription drug coverage
- A formulary of covered drugs

Certain WellCare Medicare Advantage plans could provide coverage for a diverse array of medications, potentially encompassing both brand name and generic drugs outlined in the plan’s formulary. However, some WellCare plans may impose restrictions or limitations, such as quantity limits on certain drugs, which could affect your coverage.
Potential Benefits Exclusive to WellCare
Besides providing extensive medical and prescription drug coverage, some of the WellCare Medicare Advantage plans may also offer an array of unique benefits that could provide added value and may even significantly enhance your healthcare experience, such as vision, dental, and hearing coverage.
However, what might set WellCare apart might be:
- The broad network of providers it offers
- Working in partnership with healthcare providers to develop top-notch, cost-efficient healthcare options
- Providing interactive resources to aid in managing patient conditions, possibly leading to improved healthcare outcomes.
Comparing Costs: WellCare Plans vs. Original Medicare
Cost will likely be one of the primary factors for most individuals when selecting a healthcare plan. Some of WellCare’s Medicare Advantage plans could potentially offer a cost advantage over Original Medicare in certain areas.
In terms of copays, WellCare’s plans may feature lower copays and limited out-of-pocket spending, in contrast to Original Medicare which does not have an out-of-pocket maximum. This could make WellCare’s plans a more cost-effective choice for many individuals.
When it comes to deductibles, WellCare Medicare Advantage plans may also offer some of the following benefits:
- Minimal or non-existent deductibles, potentially providing greater initial cost savings compared to deductibles under Original Medicare
- Limited annual out-of-pocket expenses
These potential features may be able to ensure that out-of-pocket expenses could be minimized for WellCare plan members.
Understanding Premiums and Copays
To assess the affordability of your health plan, it’s important to understand the associated premiums and copays. The determination of premiums and copays for WellCare’s Medicare Advantage plans will likely be based on the Member’s Benefit Plan. Each plan type, such as HMO and PPO, has different premium and copay amounts, which should be considered when assessing the overall cost of the plans.
A copayment, also known as a copay, is the payment required for a covered medical service. Some of these copay amounts may be lower than those associated with Original Medicare, possibly making WellCare’s plans a more affordable choice for many individuals.
Deductibles and Out-of-Pocket Expenses
Deductibles and out-of-pocket expenses could be another important factor to consider. The deductible amounts in WellCare’s Medicare Advantage Plans may vary significantly.
Some of WellCare’s plans may even offer the advantage of lower or no deductibles when compared to Original Medicare. Additionally, unlike Original Medicare, which does not have a limit on out-of-pocket expenses, certain WellCare plans may include a maximum out-of-pocket cap each plan year, possibly providing extra financial security for enrollees.
Enrollment Periods and Eligibility Criteria
Having explored some of WellCare’s potential offerings and their respective costs, this article shows the enrollment periods and eligibility criteria for WellCare’s Medicare Advantage plans.
To enroll in WellCare’s plans, individuals must meet certain eligibility criteria:
- They must meet the age requirement of 65 or older, or under 65 with a qualifying condition.
- They need to reside within the plan’s service area.
- They must possess Medicare Parts A and B.
When Enrollment Begins
Enrollment in WellCare’s Medicare Advantage plans begins during the Annual Election Period (AEP) or a Special Enrollment Period (SEP) for those who qualify. The Annual Election Period (AEP) for WellCare’s Medicare Advantage occurs annually from October 15th to December 7th. During this period, beneficiaries have the opportunity to transition from one Medicare Advantage plan to another.
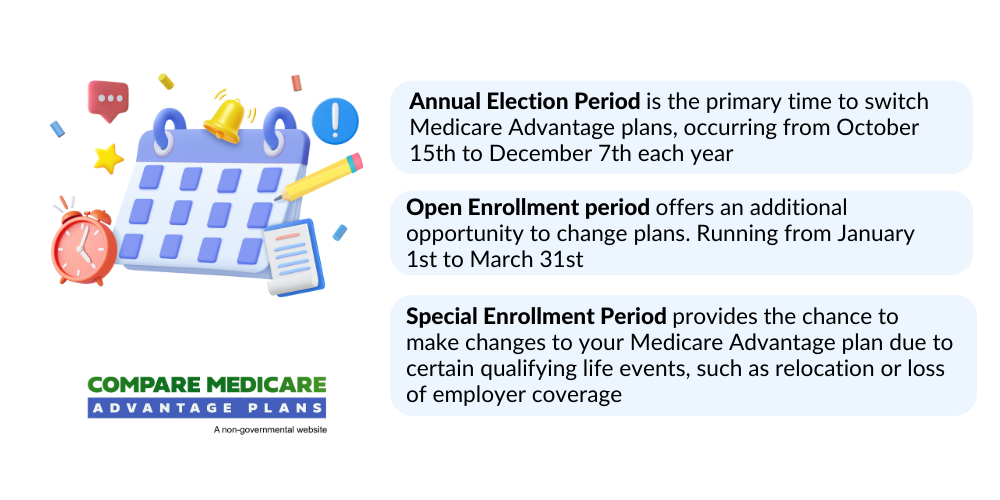
Apart from the AEP, it is also possible to transition from Original Medicare to WellCare’s Medicare Advantage during the Medicare Advantage Open Enrollment Period (MA OEP), which takes place from January 1 to March 31.
Qualifying for WellCare Medicare Advantage
To qualify for WellCare’s Medicare Advantage, individuals must meet certain qualifications. These include:
- Being at least 65 years old or under 65 with a qualifying condition
- Residing within the plan’s service area
- Possessing Medicare Parts A and B
- Being either a U.S. citizen or lawfully present in the U.S.
WellCare’s Medicare Advantage plans will likely be offered in multiple geographical regions. To be eligible, you need to be located within a service area that provides plan types such as HMO, PPO, and Special Needs Plans.
It’s important to note, however, that while it is possible to have Medicare while residing abroad, Medicare may not provide coverage for care received outside the United States. As such, permanent residence outside the U.S. could impact your coverage.
To enroll, call one of our licensed agents at 1-833-641-4938 (TTY 711), Mon-Fri 8 am-9 pm EST. They can provide comprehensive information, personalized guidance, and ongoing assistance to navigate the enrollment process for private insurance companies, making it easier for beneficiaries to make informed decisions about their healthcare.
Accessing Personal Support for Enrollment
Personal support could greatly facilitate the process of enrolling in a health plan. WellCare could provide personal support for enrollment through their Broker Support Call Center and Broker Self-Service Portal. They may also offer assistance with PPO Plans, HMO Plans, D-SNP Plans, and C-SNP Plans. It’s recommended to present your WellCare Member ID card during enrollment.
Personal support for WellCare plan enrollment is accessible from Monday to Friday, 8 a.m. to 8 p.m. Additional support may also be available on weekends for Fidelis Care Medicaid Members in New Jersey. You could reach out to WellCare’s support by contacting the Broker Support Call Center or by calling specific hotlines during their operating hours.
How to Choose the Right Plan for Your Needs
Selecting the right WellCare plan will likely require:
- Assessment of your healthcare needs
- Verification of your preferred healthcare providers’ availability within the WellCare network
- Analysis of your prescription drug needs
The right plan for you will likely depend on your healthcare needs and preferences, how often you need healthcare services, and how much you can afford to pay for these services.
Evaluating Health Care Service Needs
In assessing your healthcare needs, you might want to consider possible factors like your frequency of doctor visits, any chronic conditions you may have, and the type of healthcare services you regularly require. For example, if you have a chronic condition that requires regular checkups, you might need a plan with lower copays for office visits.
On the other hand, if you seldom need healthcare services, you might prefer a plan with a lower monthly premium.
Checking Provider Network Availability
Also, before opting for a WellCare plan, you may want to ensure that your preferred healthcare providers are included in the WellCare network. You can check this using the WellCare Find a Provider tool on their official website.
If your preferred provider is not within the network, you may want to consider whether you’re willing to change providers or whether you’d prefer to find a plan that includes your preferred provider.
Analyzing Prescription Drug Requirements
Lastly, members should contemplate their prescription drug needs. If you regularly take prescription medications, it would be beneficial to select a plan that covers your medications. You can check whether your specific medications are covered by a WellCare plan by referring to the formularies available on the WellCare website or by using their drug search tool.
Summary
Navigating the world of healthcare insurance might be daunting, but with the right information, you could make an informed decision that suits your healthcare needs and budget. Some of WellCare’s Medicare Advantage and Medicaid plans could offer comprehensive coverage options, from HMO and PPO plans to Dual Eligible Special Needs Plans.
With potential benefits such as prescription drug coverage, dental, vision, and hearing services, and access to a vast provider network, WellCare’s plans could offer a significant advantage over Original Medicare.
However, it’s crucial to understand that the best plan for you will likely depend on your healthcare needs and preferences. Therefore, take the time to evaluate your healthcare needs, check provider network availability, and analyze your prescription drug requirements before deciding. With this guide, you’ll likely be well-equipped to navigate WellCare’s potential offerings and choose the plan that best fits your needs.
Frequently Asked Questions
→ What is another name for WellCare?
WellCare is also known as Centene, which has been consolidating its Medicare options under the Wellcare brand, combining with previous brands such as Allwell, Health Net, Fidelis Care, Trillium Advantage, ‘Ohana Health Plan, and TexanPlus.
→ What’s the difference between Humana and WellCare?
The main difference between Humana and WellCare is that Humana may offer Medicare Supplement Insurance plans in addition to Medicare Part D and Medicare Advantage plans, while WellCare may only offer Part D and Medicare Advantage plans in certain areas.
→ Is WellCare Medicaid or Medicare?
WellCare will likely provide government-sponsored managed care services through Medicaid, serving families, children, and individuals with complex medical needs across numerous states.
→ What are the eligibility requirements for enrolling in WellCare Medicare Advantage?
To enroll in WellCare Medicare Advantage, you must be 65 or older, or under 65 with a qualifying condition, reside within the plan’s service area, and have Medicare Parts A and B. Meeting these eligibility requirements is essential.

ZRN Health & Financial Services, LLC, a Texas limited liability company
Russell Noga is the CEO of ZRN Health & Financial Services, and head content editor of several Medicare insurance online publications. He has over 15 years of experience as a licensed Medicare insurance broker helping Medicare beneficiaries learn about Medicare, Medicare Advantage Plans, Medigap insurance, and Medicare Part D prescription drug plans.



