

Is Medicare Primary or Secondary?
The role of whether Medicare acts as primary or secondary for you will likely hinge on specific factors such as employment, other insurance coverage, and health conditions.
This article will guide you on when Medicare could be your primary payer and when it might step in as secondary, equipping you with the knowledge to manage your coverage effectively.
Key Takeaways
- Medicare could be either primary or secondary insurance, depending on various factors like the size of the employer, type of other insurance held, and specific health situations like end-stage renal disease (ESRD).
- Medicare will likely serve as primary coverage for individuals under specific circumstances, including being over 65, working for a small business with fewer than 20 employees, or qualifying for both Medicare and Medicaid, but it could also be secondary to larger employer plans or when paired with other specific insurance policies.
- Supplemental insurance plans, including Medigap and Medicare Part D, may also play a critical role in covering additional healthcare costs not fully covered by Medicare, which could be paramount for potentially minimizing out-of-pocket expenses and ensuring comprehensive healthcare coverage.
Compare Plans in One Step!
Enter Zip Code
Determining Primary vs. Secondary Coverage with Medicare
Determining whether Medicare acts as a primary or secondary insurer will likely hinge on various factors, including the type of insurance you have, the size of your employer, and the presence of other types of insurance.
Typically, Medicare may assume the role of the primary insurer when you have multiple forms of coverage. This means that primary insurance will likely pay first for your healthcare services, paving the way for your secondary insurance to cover any remaining costs.
Medicare’s Role with Small Business Group Plans
If you work at a small business with fewer than 20 employees, Medicare may be considered your primary insurance. This arrangement means that Medicare will likely pay first for your healthcare services, followed by your employer’s group health plan. Comparing the potential cost-savings associated with this arrangement may be especially relevant for Medicare-eligible individuals.
Failing to enroll in Medicare when your employer’s coverage will likely not be considered creditable could lead to penalties, especially if both plans don’t offer the same health benefits.
Larger Employer Plans and Medicare
Working for a larger employer with 20 or more employees might change the equation. In this case, Medicare will likely take the back seat and serve as the secondary insurer to your employer’s group health plan. However, if you’re under 65 and have end-stage renal disease (ESRD), Medicare may step up to become the primary payer for your healthcare expenses.
You could also defer enrollment in Medicare Part B if you have creditable group health coverage through your employer or your spouse’s employer.
Coordination of Benefits: How Medicare Interacts with Other Policies
In terms of coordinating potential benefits, Medicare and other insurance policies will likely have to strike a delicate balance. The ‘coordination of benefits’ rules may ensure that Medicare and other policies follow the correct payment order. For instance, if you have both Medicare and retiree health coverage, Medicare typically pays first, and your retiree health plan may play the role of the secondary payer.
In complex cases involving multiple payers, these rules may also dictate the sequence of payment.
Medicare’s Position When Paired with Specific Insurances
When Medicare plays with specific insurances such as:
- disability
- COBRA
- TRICARE
- retiree coverage
- health insurance (e.g., Medicaid)
The rules of the game may change. The type of insurance you have in conjunction with Medicare will likely influence whether Medicare is to pay as the primary payer or take the back seat as the secondary payer.
Medicare and Disability Insurance
For disabled individuals under 65, Medicare will likely act as the primary payer, with disability insurance playing the secondary role. Once you qualify for Social Security Disability benefits, you may receive Medicare after a waiting period, making it the primary coverage.
However, your employer-based health plan may serve as secondary insurance if the employer has fewer than 100 employees and may not be part of a federal health insurance program.
The Intersection of Medicare and COBRA
Navigating the intersection of Medicare and COBRA might be complex. Medicare will likely assume the role of the primary payer when you’re also covered by COBRA. However, there may be exceptions. For instance, if you have End-Stage Renal Disease (ESRD), COBRA coverage could potentially be primary for a 30-month coordination period.
Working with TRICARE: Military Members and Medicare
For military members and their families, TRICARE and Medicare may also work together to ensure comprehensive coverage. If you’re retired military personnel over the age of 65, Medicare will likely act as the primary payer, with TRICARE stepping in to cover additional costs.
Enrolling in a Medicare Advantage plan could also provide supplementary benefits such as dental and vision coverage.
Retirement and Health Coverage: Medicare’s Primacy
Upon retirement, the healthcare coverage landscape could change dramatically. Typically, Medicare steps up as the primary payer, while your retiree health plan might take a secondary role. This arrangement means that Medicare could pay first for your healthcare services, followed by your retiree health plan.
This coordination between retiree insurance and Medicare could potentially provide comprehensive coverage, possibly ensuring that you’re not left with unexpected expenses when it comes to your healthcare needs.
Dual Coverage: Medicare and Medicaid Together
If you’re one of the millions of Americans who qualify for both Medicare and Medicaid, you’re considered dual-eligible. In this case, Medicare could serve as the primary payer, and Medicaid may act as the secondary payer.
This dual coverage could help you cover a wide range of healthcare services, from preventive care under Medicare to long-term services and supports (LTSS) under Medicaid.
Navigating Medicare with Special Health Situations
Special health situations like end-stage renal disease (ESRD) and workers’ compensation may also add another layer of complexity to the Medicare puzzle. Understanding how Medicare might interact with these unique circumstances could help you navigate your healthcare coverage more effectively.
ESRD Patients: Understanding Medicare’s Primary Role
Individuals grappling with end-stage renal disease (ESRD) may rely on Medicare as their primary payer, regardless of any other health coverage they may have.
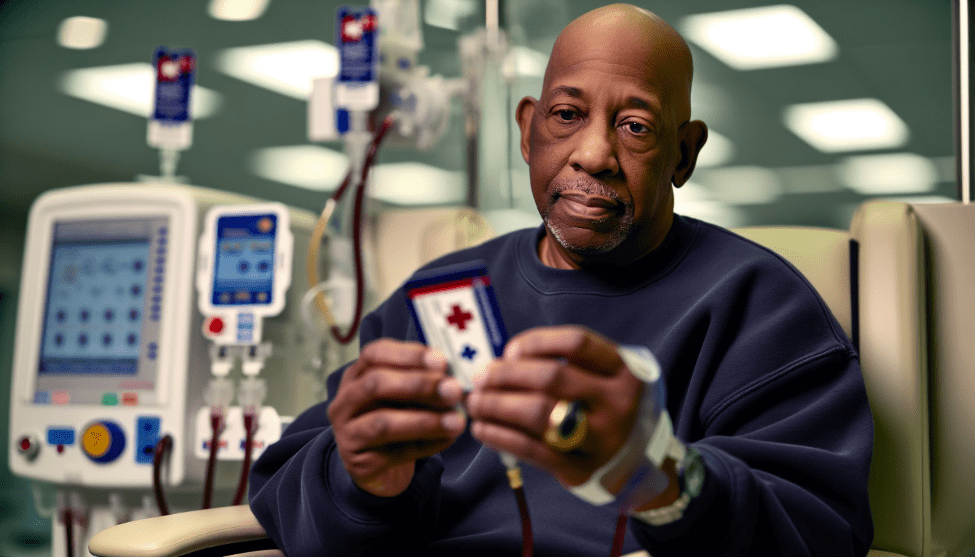
This could potentially ensure they could get access to the necessary medical care and treatments. In this case, Medicare will likely take the lead in paying for healthcare services, with other insurance coverage following suit.
Understanding how Medicare might coordinate with other insurance could help ensure that ESRD patients receive optimal healthcare coverage.
Workers’ Compensation and Medicare: Who Pays First?
In cases involving workers’ compensation, the compensation plan might play the role of the primary payer, with Medicare acting as the secondary payer. When filing a worker’s compensation claim, Workers’ Compensation may also cover the healthcare services related to the accident or injury, with Medicare stepping in afterward.
Understanding how these two entities, including a federal healthcare provider, interact could help ensure that you receive comprehensive coverage for your healthcare needs.
Supplementing Medicare: Secondary Plans and Their Benefits
Supplementing Medicare with secondary plans like Medigap and Medicare Part D could potentially help cover additional healthcare costs. Some of these supplemental plans may serve as secondary payers, possibly providing coverage for healthcare costs not fully covered by Medicare.
Understanding these Medicare supplement insurance plans, their potential benefits, and their role in your healthcare coverage could help you maximize your coverage and potentially minimize out-of-pocket expenses.
Medigap: Bridging the Gap in Medicare Coverage
Medigap will likely help bridge the gap in Medicare coverage. As a secondary payer to Medicare, Medigap might cover expenses that Medicare doesn’t cover, such as copayments, coinsurance, and deductibles.
Grasping the various Medigap plans and their potential benefits could enable you to maintain comprehensive healthcare coverage that suits your requirements while managing medical costs.
The Role of Medicare Part D in Prescription Coverage
Medicare Part D may serve as the primary payer for prescription drugs, possibly helping to reduce drug costs and safeguard against elevated expenses. However, secondary insurance could also play a significant role in reducing the expenses that may be associated with certain Part D-covered drugs, particularly during the coverage gap, also known as the donut hole.
Comprehending the interaction between Medicare Part D and secondary insurance will likely enhance your prescription drug coverage.
Medicare and Other Federal Programs: Understanding Priority
Coordinating Medicare with other federal programs such as VA benefits and Black Lung benefits may also add another layer of complexity to understanding your healthcare coverage. Familiarizing yourself with how these programs work with Medicare could be crucial for comprehensive healthcare coverage.
Medicare and VA Benefits Coordination
If you’re a veteran who qualifies for both Medicare and VA benefits, navigating your healthcare coverage might be a bit complex. While both Medicare and VA benefits could act as primary coverage, certain VA benefits might take precedence for treatment received through VA channels.

On the other hand, Medicare may be primary for healthcare services received outside of the VA system.
Black Lung Benefits: Where Does Medicare Stand?
The Federal Black Lung Program is a federal initiative that has been designed to offer monthly payments and medical benefits to coal miners who have been completely disabled due to black lung disease acquired from working in the country’s coal mines.
If you qualify for this program, it may serve as the primary payer for specific treatments associated with black lung disease, with Medicare acting as the secondary payer.
Legal Framework of Medicare as a Secondary Payer
The Medicare Secondary Payer Act may also significantly influence Medicare’s role as a secondary payer. Understanding this legal framework could help ensure that you’re receiving the appropriate coverage from your primary insurer and that Medicare has been correctly coordinated as a secondary payer.
Maximizing Your Coverage: The Importance of Secondary Insurance with Medicare
Securing secondary insurance with Medicare will likely be pivotal for optimal healthcare coverage. Secondary insurance may cover expenses that Medicare doesn’t, such as copayments, coinsurance, and deductibles, potentially reducing your out-of-pocket costs and providing additional coverage for covered services not included in Medicare coverage.
How Medicare Advantage Fits Into the Equation
Medicare Advantage will likely fit into the primary-secondary insurance equation, by acting as the primary coverage. With a Medicare Advantage plan, the private insurance company, rather than Medicare, may pay for your medical care.
Some of these plans may offer additional benefits not covered by Original Medicare, helping to ensure that you have comprehensive healthcare coverage.
Summary
Understanding Medicare’s role as a primary or secondary insurer could be crucial for navigating your healthcare coverage effectively. From employer plans and specific insurance policies to special health situations and other federal programs, the landscape of Medicare coverage might be complex.
However, with the right knowledge and understanding, you could potentially ensure that you’re making the most of your Medicare coverage.
Frequently Asked Questions
→ Is Medicare the primary or secondary?
Medicare will likely be the primary insurance, but in some cases, a supplement to Medicare may be secondary, especially if you have job-based insurance from an employer with 20 or more employees. This might make Medicare the primary payer for beneficiaries not covered by other types of health insurance.
→ How do you determine which health insurance is primary?
To determine which health insurance is primary, you should consider that the plan under your employer may be primary, while a spouse’s or parent’s plan would be secondary if you are covered under both. This means that your plan will likely be primary if you have coverage under a plan from your employer in addition to a spouse’s or parent’s plan.
→ Can you have Medicare and employer insurance at the same time?
Yes, you could have both employer insurance and Medicare at the same time, and the coverage may be able to work together to help you access necessary care without incurring high costs.
→ Who pays medicare?
Medicare will likely be funded through a combination of general revenues, payroll taxes, and premiums paid by beneficiaries. Taxpayers, employees, and employers may also contribute to funding Medicare through payroll taxes.
→ How does Medicare interact with disability insurance?
Medicare will likely serve as the primary payer for disabled individuals under 65, with disability insurance acting as the secondary payer. This means that Medicare might cover medical expenses first before disability insurance kicks in.

ZRN Health & Financial Services, LLC, a Texas limited liability company